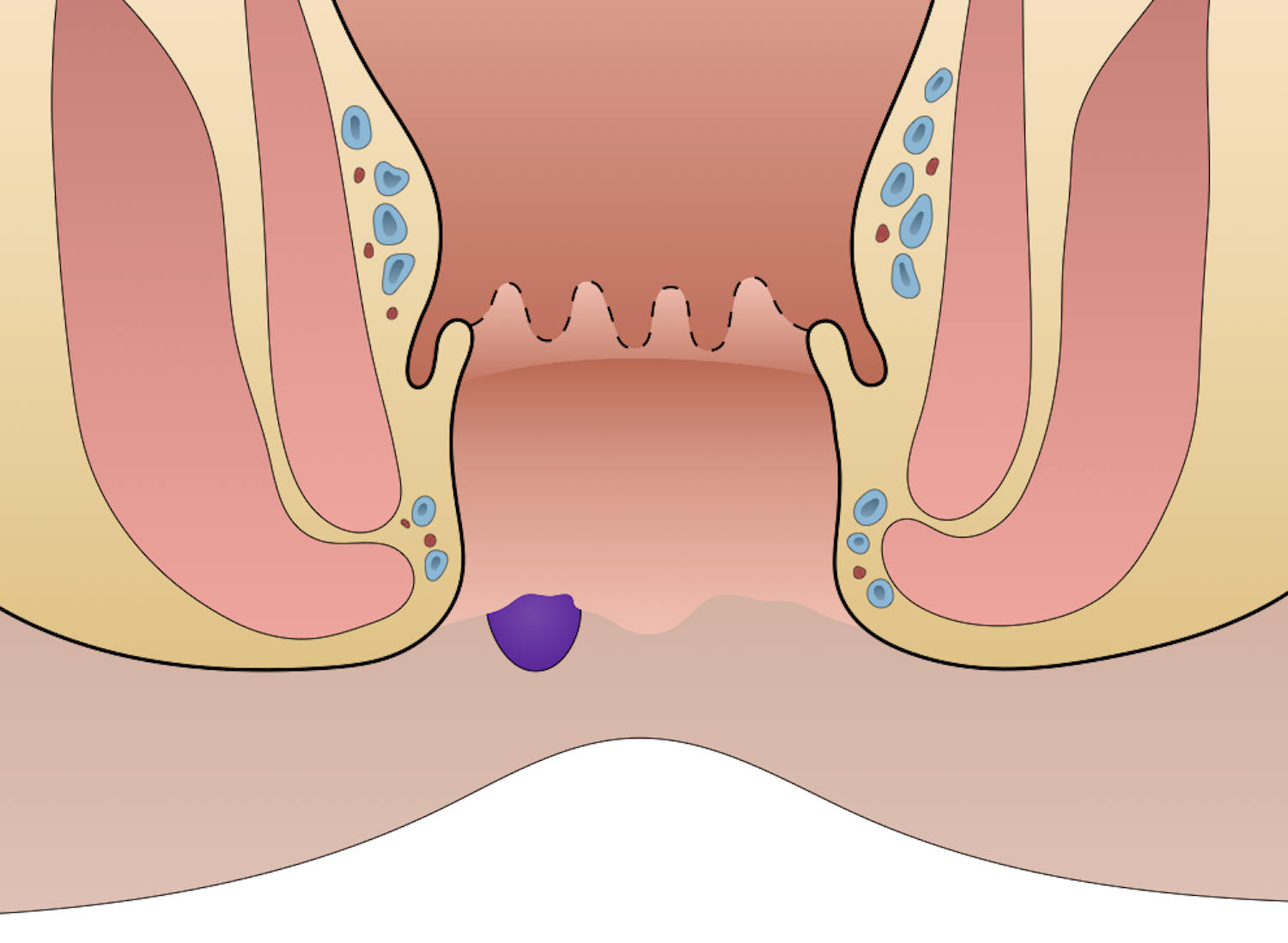
External hemorrhoids occur distal to the dentate line. The treatment of hemorrhoids in the past has included suppositories, cautery, and excision. Walter Whitehead introduced a radical procedure in 1882 in which most of the area involved with the hemorrhoid was excised. Since 1882, additional approaches have come about. Notably, from Edward Campbell Milligan, James Morgan, and James A. Ferguson, among others.
Etiology
- Straining
Pathogenesis
- Increased intraanal pressure leads to abnormal dilatation and engorgement of vascular channels
- Changes in the connective tissue within the anal cushions occurs as a result
- These changes cause an inflammatory reaction and vascular hyperplasia, which can be evident in hemorrhoids
- When the tissue that usually supports hemorrhoids fails, the anal cushion is displaced sitally and undergoes venous distention, erosion, bleeding, thrombosis, and/or tissue prolapse
History
- Anal itching
- Anal pain
- Rectal bleeding
- Thrombosed external hemorrhoid
- Acute onset severe anal pain
- Pain may be worsened by sitting or defecation
- May be preceded by an episode of constipation or diarrhea
- Usually resolves with conservative treatment within 72 hours after symptom onset
Physical Exam
- Rectal bleeding
- Thrombosed external hemorrhoid → nonreducible lump at anal verge
- Digital rectal exam
- Anoscopy
Treatment
- Conservative treatment
- Increased fiber intake
- Increased fluid intake
- Sitz bath
- Lidocaine ointment
- Stool softeners
- Surgical removal if pain is excessive or failure to respond to conservative treatment
- Thrombectomy with evacuation of clot without skin closure
- May be completed if patient presents within the first 72 hours with symptoms. No advantage after 1 week unless the patient is continuously bleeding or has extensive inflammation.
- Allows for quicker symptom resolution
- Excisional hemorrhoidectomy
- Decreased chance of recurrence
- Faster resolution of symptoms
- Indications
- Symptomatic combined internal and external hemorrhoids with prolapse (grades III – IV)
- Substantial associated skin tags
- Techniques
- Closed (Ferguson) hemorrhoidectomy
- Most commonly used technique
- Closes the mucosa with sutures after hemorrhoid tissue removal
- Associated with less postoperative pain, faster healing, and reduced risk of postoperative bleeding compared to open (Milligan-Morgan) hemorrhoidectomy
- Open (Milligan-Morgan) hemorrhoidectomy: leaves mucosa open
- Closed (Ferguson) hemorrhoidectomy
- Thrombectomy with evacuation of clot without skin closure
- Rule out colon cancer with colonoscopy
Relevant Information
- History should be taken to include issues of perineal hygiene, fiber intake, bowel habits, including frequency, consistency, change in stool caliber, difficulty with evacuation, fecal incontinence
- Dentate line (pectinate line): demarcates superior ⅔ of anal canal from inferior ⅓; embryologic landmark


Complications
- Skin tags
- Strangulated hemorrhoids
Differential Diagnoses
- Colon cancer
- Anal fissure
- Anorectal abscess
- Anal prolapse
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Management of Hemorrhoids,” (2024)