Amputation is the loss or removal of a body part. Prehistoric bones show that man was performing amputations at the prehistoric time by utilizing cutting instruments. In 1915, E. Holländer performed an amputation using neolithic-age tools within six or seven minutes. In the first century A.D., incisions were made in healthy tissue, circular flap amputations were made, and ligatures were used to control bleeding. In the sixteenth century, amputations entered the modern era.
Indications
- Trauma
- Vascular supply issues (most common indication for amputating the lower extremity is an inadequate blood supply, often after failure of a vascular bypass graft); necrosis
- Malignant neoplasm
- Chronic osteomyelitis
- Life-threatening infections
- Inoperable congenital limb deformity in children
- Emergency amputations: systemic complications or extensive infection
Contraindications
- Patients not medically stable enough to survive surgery/anesthesia
- Localized skin infections → delay amputation if possible
Preoperative Considerations
- Selection of amputation level should consider objectives of removing all nonviable tissue while ensuring primary wound healing and a functional result. The amputation level should fulfill the following criteria:
- Palpable pulse immediately proximal to level of amputation
- Skin perfusion pressure > 20 mmHg is predictive of primary amputation healing
- Trauma: evaluate extent of tissue and vascular damage in terms of possibly preserving the extremity
- IVF and colloid solutions: shock
- Control chronic diseases like diabetes or advanced vascular disease
Relevant Anatomy
- Greater saphenous vein and nerve are in the subcutaneous tissue of the medial thigh. Lesser saphenous vein is in the subcutaneous tissue of the posterior leg and runs parallel to the sural nerve.
- Profunda femoral artery (deep femoral artery)
- Usually arises from posterolateral aspect of femoral vein
- Tends to be the main channel after occlusion of the superior femoral vessels or a femoral-popliteal bypass graft

- Pes anserine (“goose’s foot” in Latin): conjoint tendon of sartorius, gracilis, and semitendinosus where they insert on anteromedial proximal tibia
- Popliteal artery
- Continuation of femoral artery
- Exits popliteal fossa under soleus muscle
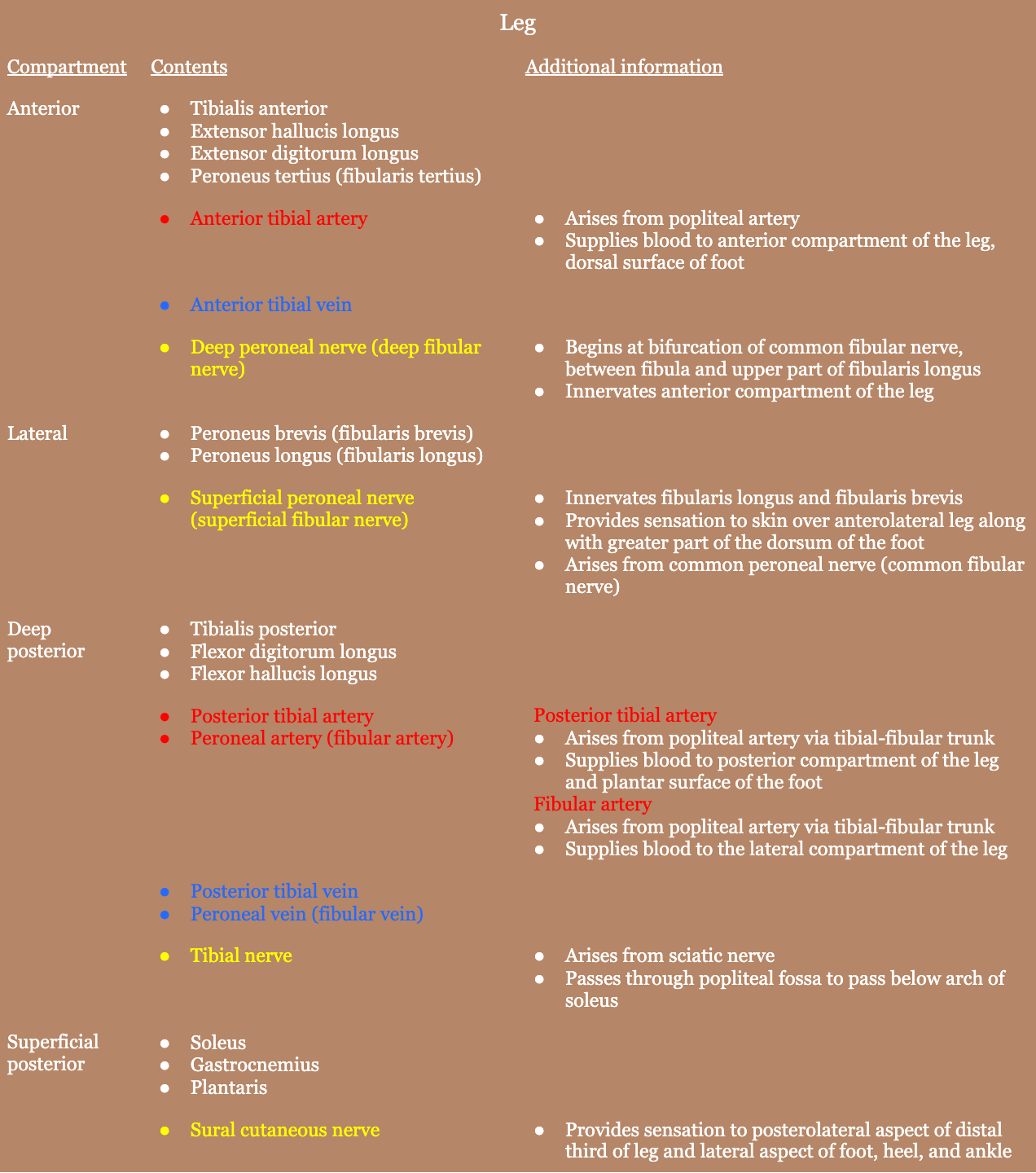
- Lower extremity nerves
- Obturator nerve: hip adduction
- Superior gluteal nerve: hip abduction
- Inferior gluteal nerve: hip extension
- Femoral nerve: knee extension
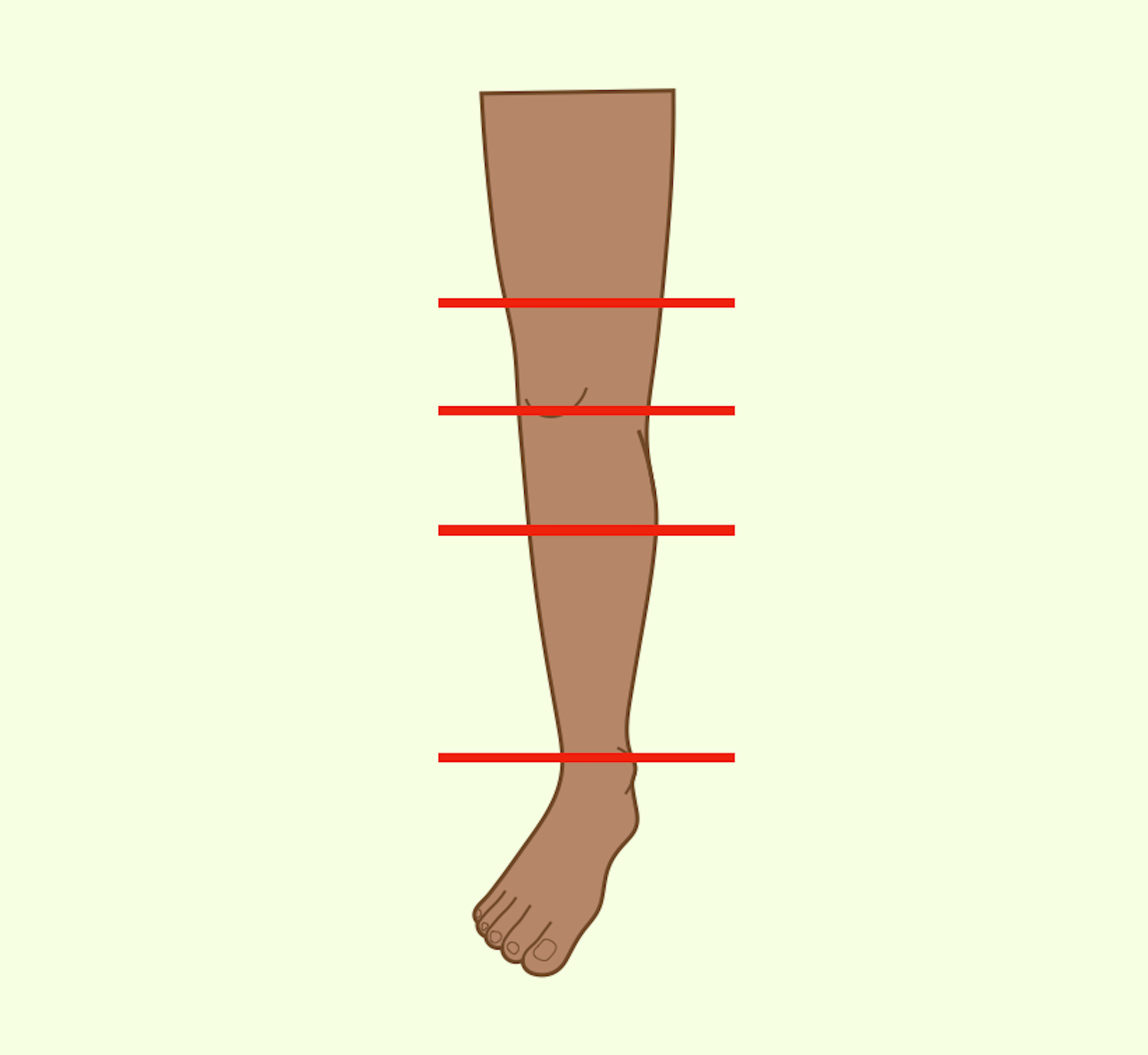
Relevant Information
- Amputation types
- Above-knee amputation (AKA)
- Supracondylar amputation: distal femur
- Diaphyseal amputation: midfemur
- High above-knee amputation: just below lesser trochanter
- Through-knee amputation
- Below-knee amputation (BKA)
- Types
- Open below-knee amputation:
- Formal below-knee amputation
- At least 8 cm of tibia (from tibial tuberosity) should be preserved for prosthesis
- > 20 cm is probably not any more functionally effective
- A very short fibula tends to migrate laterally and may be removed in a short below-knee stump
- Types
- Ertl amputation: an osteomyoplastic procedure for transtibial amputation
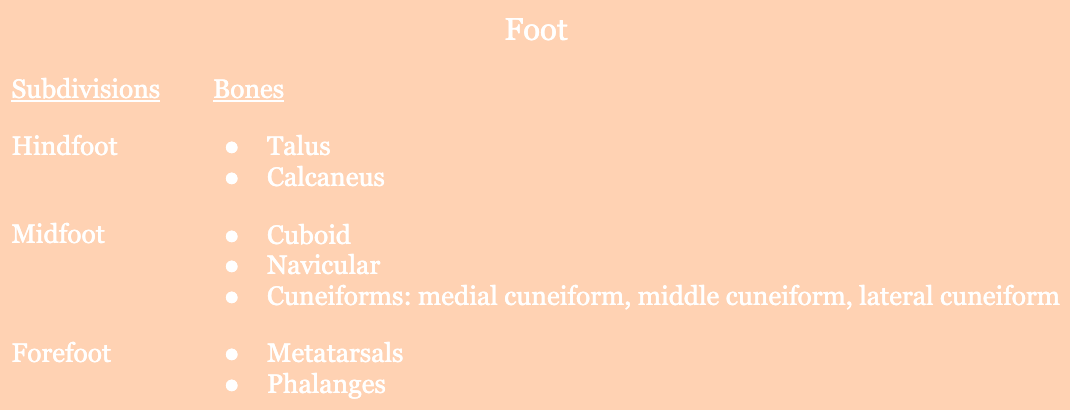
- Ankle and midfoot amputations
- Syme amputation
- Weight-bearing amputation through the ankle
- Removal of all bones of the foot, while preserving the heel pad in order for weight-bearing
- Boyd amputation
- Weight-bearing amputation through ankle
- Preserves calcaneous and heel pad-for weight bearing
- Calcaneus is fused with tibia and is non-mobile
- Syme amputation
- Foot amputations
- Chopart amputation
- Weight-bearing amputation between navicular/cuboid bones and the talus/calcaneus bones
- Preserves additional length of the foot
- Transmetatarsal amputation
- Weight-bearing amputation at the level of the metatarsal shafts
- Preserves additional length of the foot
- Preferable to amputation through the hindfood or BKA
- Chopart amputation
- Above-knee amputation (AKA)
- Flap types
- Scar placement
- Upper extremity: posterior of the stump (since prosthesis bears largely on distal surfaces of the stump)
- Lower extremity: away from areas of direct pressure
- Fingers/toes: use long palmar and plantar flaps to cover the stump with thick, protective tissue pad; Racket incision is recommended for toes since they may extend upward to expose the metatarsals or may be used for amputations of digits where all possible length must be preserved (especially thumb)
- Scar placement
- Due to the anatomy of the profunda femoral artery, the amputation is usually above the knee. The supracondylar amputation is the most frequent site for amputation in the presence of arterial insufficiency (though a below-knee amputation is preferable, if possible).
- Knee disarticulation and supracondylar amputation yields a stump that can be difficult to fit with a prosthesis. A short BKA is preferable to a knee disarticulation.
- Generally speaking, as much length should be saved as possible, except, perhaps, for below-knee amputations. This is because the anterior tibia prevents a pressure point at the stump which means there must be enough solid tissue with good blood supply to cover it. So it needs a long posterior flap to be transposed anteriorly completely over the stump.
Surgical Technique
- In the absence of infection, the leg is elevated to encourage venous drainage prior to tourniquet application. Tourniquets are not used in cases of atherosclerosis due to the possibility of damaging blood vessels to the stump.
- Tourniquet is above the elbow (to control brachial artery) for major amputations of the forearm
- Tourniquet is placed above the knee for lower leg and foot amputations
- Tourniquet is placed high in the thigh for knee and lower thigh amputations
- Extremity is prepped and draped in the usual sterile fashion. It can be elevated with sterile towels as needed.
- Arteries and veins should be tied individually.
- Nerves are divided with nonabsorbable sutures at as high a level as possible and buried within muscle to prevent neuroma formation. The nerves should be away from the scar and any areas of pressure, as neuromas become symptomatic when pressure is applied.
- Bone is divided at the appropriate level to permit the soft tissue to approximate and produce a thick covering for the stump. Sharp margins of the bone are beveled with rongeur or rasp.
- Hemostasis is achieved and a closed-suction drain may be placed if needed for larger amputations. Investing fascia is loosely approximated with interrupted absorbable suture.
- If a guillotine “drainage” type of amputation was used, the wound is left open and closed secondarily later, or reamputated at a later date.
Postoperative Complications
- Muscle atrophy
- Wound complications
- Infection
- Wound dehiscence
- Seroma
- Hematoma
- Risk factors: sepsis, compartment syndrome, ESRD, tobacco use, BMI > 30, BKA
- Phantom limb pain
- Depression
- Anxiety
- Death