Anorectal (perirectal) abscesses are usually the result of an infection of the anal glands located at the dentate line. They commonly expand caudally to the anoderm (perianal abscess) or across the external sphincter into the ischiorectal fossa (ischiorectal abscess).
Etiology
- Nonspecific: cryptoglandular
- Inflammatory
- Crohn disease
- Tuberculosis
- Actinomyces
- Lymphogranuloma venereum
- Traumatic
- Impalement
- Foreign body
- Anal fissure
- Iatrogenic
- Episiotomy
- Hemorrhoidectomy
- Prostatectomy
- Radiation
- Malignancy
- Rectal or anal carcinoma
- Leukemia
- Lymphoma
Epidemiology
- Occur more often in males
- Peak incidence among 20 – 40 year olds
Pathogenesis
- The abscess will commonly undergo caudal expansion to the anoderm (perianal abscess) or across the external sphincter into the ischiorectal fossa (ischiorectal abscess)
- Perianal abscesses
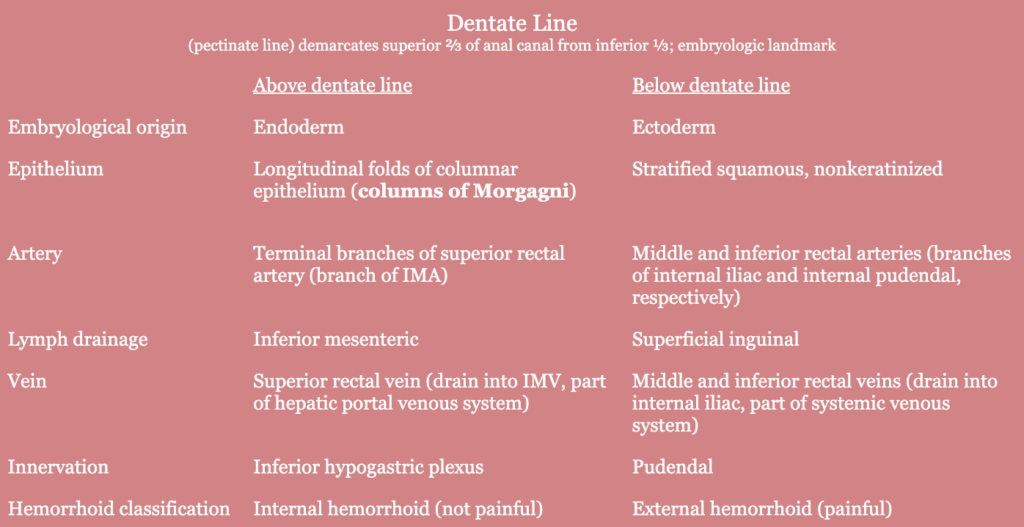
- Usually result from an infection of the anal glands, located at the level of the dentate line
- Attributed to an obstruction of the draining duct from fecal debris (“cryptoglandular abscess”)
- Obstruction of the ducts leads to stasis, bacterial overgrowth, and ultimately results in an abscess in the intersphincteric space
History
- Indolent onset of constant, throbbing pain in the perianal/perirectal region
- Pain associated with localized swelling, erythema, and fluctuance
- Pain worsened with sitting and defecation
- ± Fever, chills, malaise
- Supralevator abscess
- Lower back pain
- Dull ache in pelvic region
Physical exam
- Erythema, induration, and fluctuance of perianal/perirectal region
- Spontaneous drainage
- Digital rectal exam: perianal/rectal submucosal mass/fluctuance
Labs
- ± Leukocytosis
- ± Elevated neutrophils
- ± Elevated lactate
Imaging
- Obtained if diagnosis is in question
- CT pelvis (often with triple contrast)
- Obtained in patients with significant comorbidities, complex anorectal conditions, and when surgical consultation isn’t immediately available
- Finding: oval-shaped fluid collection with an enhancing wall, with or without demonstration of air
- Exam under anesthesia
- Evaluate patients with recurrent or bilateral abscesses for intraoperative drainage, including cases where internal drainage may be necessary
- MRI
Treatment
- Incision and drainage, under local or general anesthesia
- External I&D through the skin
- For perianal, superficial, intersphincteric, and ischiorectal abscesses
- All are below the levator muscles
- Steps
- Drainage starting at the most fluctuant aspect of the abscess, staying as close to the anus as possible to shorten the length of any subsequent fistula track
- Probe the cavity with the examining finger or instrument to assess the extent of the cavity
- A cruciate incision with subsequent removal of the corners is a reliable way to assure adequate drainage of the entire cavity. Aggressive digital disruption of loculations should be avoided as it may injure the sphincter complex or pudendal nerve.
- If the abscess cavity is > 5 cm, the surgeon may consider placing counterincisions and bridging them with penrose drains to avoid large gaping perineal wounds that may result in prolonged healing, scarring, and distortion of the anatomy. An alternative method may include a drainage catheter that can be left in place until the abscess resolves.
- Packing the abscess cavity is a common practice, but is usually unnecessary. It may be necessary in selected patients to provide hemostasis.
- Internal I&D with transanal approach
- For supralevator and deep intersphincteric abscesses
- External I&D through the skin
- Antibiotics are usually only considered in high-risk patients (e.g., immunosuppression, diabetes, extensive cellulitis, prosthetic devices, high-risk cardiac, valvular, and related anatomical conditions) or in patients with signs of infection
- Biopsy is done to rule out anal cancer
Relevant Information
- Anal canal: connection between the anal verge and anorectal junction; 2 – 4 cm in length
- Anal crypts are located between the columns of Morgagni, where anal ducts empty
- Ischiorectal/ischioanal fossa
- Pyramidal shaped potential space between perineum and levator ani
- Medial: levator ani and external sphincter
- Lateral: obturator internus muscle and fascia
- Anterior: transverse perineal muscles
- Posterior: gluteus maximus and sacrotuberous ligament
- 30% develop fistula-in-ano
Complications
- Fistula formation
- Bacteremia/sepsis
- Fecal incontinence
- Urinary retention
- Constipation
- Recurrence
Classifications
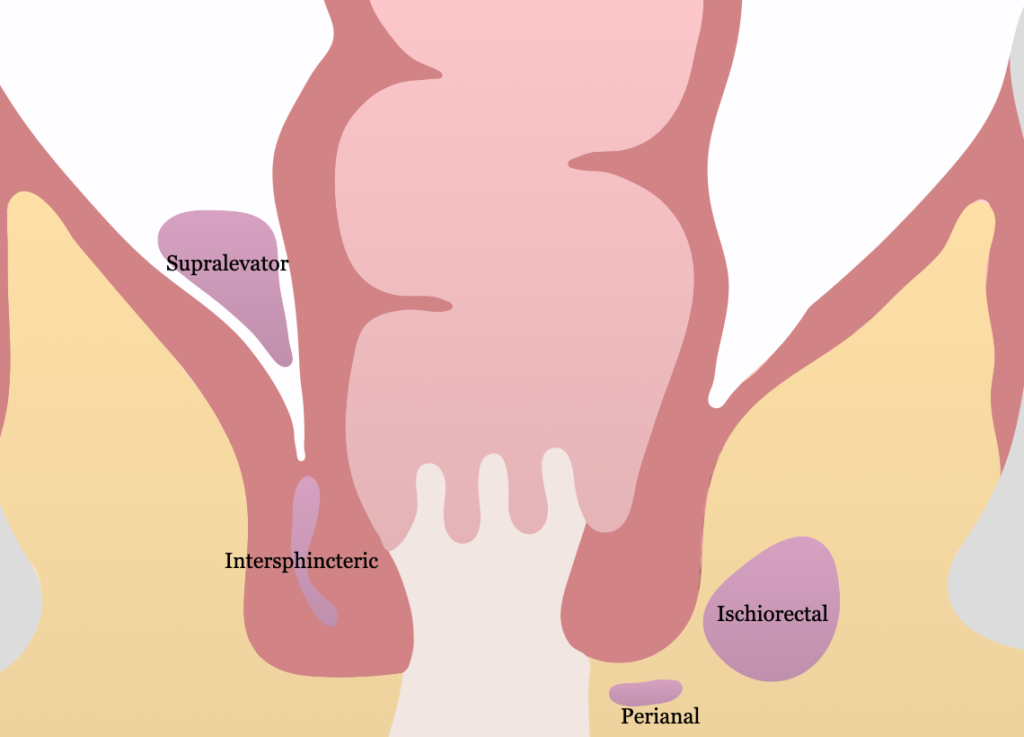
- Anorectal abscesses are named according to the potential space it is located in
- Perianal abscess (most common)
- At anal verge; confined to perianal space
- Can extend into ischioanal space or intersphincteric space
- Ischiorectal (ischioanal) abscess: between rectal wall and pubic tubercle
- Supralevator and intersphincteric abscess
- Submucosal abscess
- Perianal abscess (most common)
- Horseshoe abscess
- Large abscess in postanal space that extends bilaterally to ischiorectal fossa
- Can be formed by intersphincteric and ischiorectal abscesses
Differential Diagnoses
- Anal fissure
- Thrombosed external hemorrhoid
- Levator spasm
- Sexually transmitted infections
- HIV
- Inflammatory bowel disease, specifically Crohn disease
- Pilonidal cyst
- Hidradenitis suppurativa
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula,” (2022)
