Cholecystectomy is the surgical removal of the gallbladder. The first cholecystectomy was performed by Carl Langebuch in 1882. Prior to the first cholecystectomy, symptoms of gallstones were treated with drainage and stone extraction. Erich Mühe performed the first laparoscopic cholecystectomy in 1985.
Indications
- Acute calculus cholecystitis
- Symptomatic cholelithiasis
- Acalculous cholecystitis
- Gallstone pancreatitis
- Biliary dyskinesia
- Gallbladder masses and polyps concerning for malignancies
Preoperative Considerations
- Converting to open
- Scar tissue making dissection difficult
- Unclear anatomy
Preoperative Preparation
- Documentation of the diagnosis of biliary disease with RUQ US
- CXR, as indicated
- EKG, as indicated
- Routine lab testing, including LFTs
Risks
- Bleeding
- Infection
- Trocar injuries to viscera/blood vessels
- Bile duct injury
Relevant Anatomy
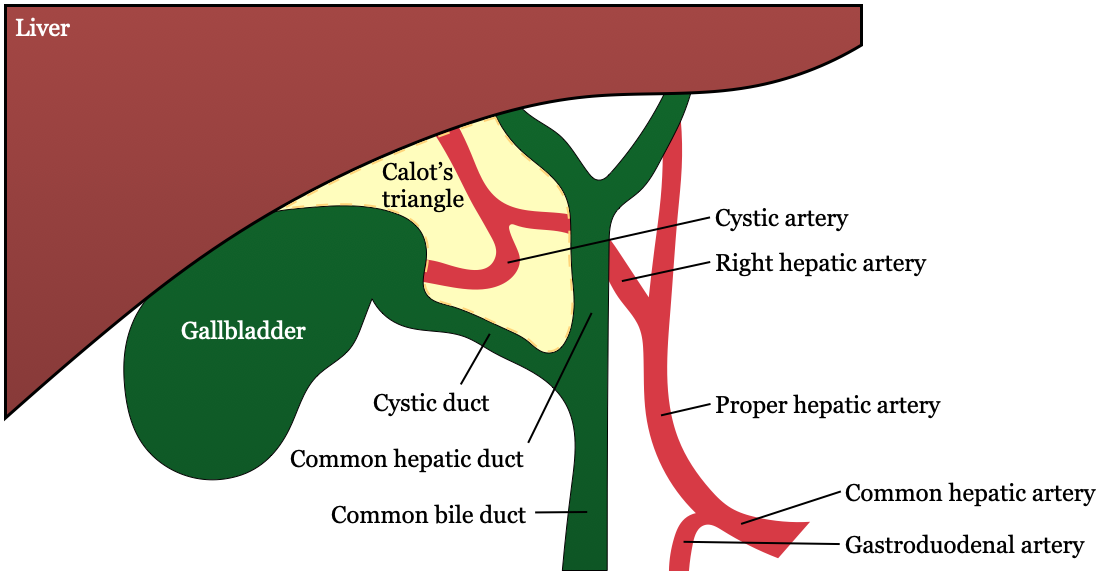
- Common bile duct → cystic duct + common hepatic duct
- Cystic artery originates from R hepatic artery
- Triangle of Calot (hepatocystic triangle): most common path of cystic artery to GB; contains Cystic artery
- Cystic duct (laterally)
- Common hepatic duct (medially)
- Liver edge (superiorly)
- Sentinel lymph node of GB resides in triangle, known as Lund’s node
- Critical view of safety (Strasberg’s method)
- Two structures connected to GB: cystic duct (lateral) & cystic artery (medial)
- Lower ⅓ of GB separated from liver to expose cystic plate → a flat ovoid fibrous sheet located in the gallbladder bed; it is a part of sheath/plate system of the liver and continuous with liver capsule
- Hepatocystic triangle (aka Calot’s triangle) is completely clear
- The round ligament of the liver (or ligamentum teres, or ligamentum teres hepatis) is a ligament that forms part of the free edge of the falciform ligament of the liver. It connects the liver to the umbilicus. It is the remnant of the left umbilical vein.
- Ducts of Luschka: small ducts that drain bile into the GB from the liver
- R hepatic artery is susceptible to injury during cholecystectomy because of proximity to Calot’s triangle
Relevant Information
- Physiology
- Source of alkaline phosphatase: bile duct epithelium (alk phosph will be elevated in bile duct obstruction)
- Bile
- Composition: cholesterol, lecithin (phospholipid), bile acids, bilirubin
- Function: emulsifies fat
- Enterohepatic circulation: circ of bile acids from liver to gut & back to liver
- Most bile acids are absorbed in terminal ileum
- GB emptying is stimulated by cholecystokinin (stimulated by fat and protein ingestion; made by duodenal mucosal cells) & vagal input
- Pathophysiology
- Patient gets jaundice with T bili of 2.5, usually first able to see under the tongue
- Obstructive jaundice S&S: jaundice, dark urine, clay-colored stools, pruritus (d/t bile salts in the dermis → not bilirubin!), loss of appetite, nausea
- Klatskin tumor: cholangiocarcinoma of bile duct at the junction of R & L hepatic ducts
Surgical Technique
- Skin of the entire abdomen and lower chest is prepped and draped in the usual sterile fashion.
- The liver is palpated, with the patient in mild Trendelenberg position, and an appropriate site is selected for the creation of pneumoperitoneum. After the camera is prepped and the intra-abdominal organs are inspected for trocar-related injuries, three additional trocars are placed under direct visualization.
- The second 10-mm (or 5-mm) trocar is placed in the epigastrium about 1-2 cm below the xiphoid, with its intra-abdominal entrance site being to the right of the falciform ligament.
- Two smaller 5-mm trocars are placed (these will be used for instruments): one in the RUQ near the midclavicular line several centimeters below the costal margin; the other very lateral almost at the same level as the umbilicus
- Ratcheted forceps are used to grasp the apex of the gallbladder fundus and then the gallbladder and liver are lifted superiorly in order to provide exposure of the undersurface of the liver and gallbladder.
- The infundibulum of the gallbladder is grasped with forceps through the middle port and, with lateral traction, the region that contains the cystic duct and cystic artery, are exposed. Dissecting forceps or hook cautery are inserted into the subxiphoid port to open the peritoneum over the junction of the gallbladder and cystic duct. From here, the cystic duct and cystic artery are exposed circumferentially and, if possible, dissected freely and identified prior to clipping and division. [critical view of safety] Division of the peritoneum to the right of the infundibulum and cystic duct may be helpful for intiital dissection and could help minimize risk of blind dissection close to the area of the common bile duct.
- The window can be verified by passing an instrument through the space. If dissection is difficult due to swelling or scarring, consider converting to an open procedure. If anatomy is unclear, consider an intraoperative cholangiogram.
- The cystic artery is cleared for a 1-cm zone and followed to the surface of the gallbladder and the clear zone is secured with metal clips proximally and distally. The cystic artery can then be divided with endoscopic scissors. The cystic duct is also cleared for about 2-cm or so in order for the surgeon to clearly identify its continuity with the gallbladder and achieve the critical view of safety. A metal clip is applied ass high as possible on the cystic duct where it begins to dilate and form the gallbladder.
- If no cholangiogram is performed, two clips are placed on the proximal cystic duct and the duct is divided.
- If cholangiogram is performed, the cystic duct is opened and bile is noted. The opening can be dilated if necessary with scissor tips and then the cholangiogram catheter is passed through the middle port or through a 14-gauge angiocath into the abdominal wall between the midclavicular trocar and the anterior axillary line. The duct is cannulated and catheter is secured. The camera and metal instruments are removed and radiolucent ports are aligned in a vertical axis to minimize their appearance on x-ray. The surgical field is covered with a towel for x-ray equipment to be positioned. Simple dye injections under fluoroscopy are performed and the principal ducts are visualized in order to ensure anatomic integrity, the absence of ductal stones, and flow into the duodenum.
- In the cholangiogram is abnormal/confusing, teh surgeon should convert to open with full anatomic verification. If choledocholithiasis is identified, the surgeon may choose to perform laparoscopic CBD exploration or complete the cholecystectomy and plan for post-op ERCP.
- Upon completion of satisfactory cholangiogram, cystic duct is doubly clipped and divided. The cystic duct-gallbladder junction is grasped with forceps through the middle port and the gallbladder is removed from its bed beginning inferiorly and progressing up to the gallbladder fossa. Most surgeons will score the lateral peritoneum with electrocautery for a centimeter and then elevate the gallbladder from the liver bed. The surgeon should reinspect the clips placed earlier in the case for slippage and inspect the liver bed for bleeding. Final peritoneal attachments of the gallbladder are divided from the liver, which will cause the liver to fall back to its anatomic position.
- The camera is removed from the umbilical port and placed in the epigastric. If there are concerns for gallbladder malignancy, infection, or spillage, a bag may be used to remove the gallbladder. Grasping forceps are placed through the umbilical port to pick up the end of the gallbladder near the cystic duct (or bag).
- After removal of the gallbladder, the camera is used for a final inspection of the abdomen. All ports are removed and sites are inspected for bleeding. The camera is removed and pneumoperitoneum is evacuated to reduce postoperative discomfort. Port sites are closed with glue.
Postoperative Complications
- Hemorrhage
- Infection
- Bile duct injuries
- Post-cholecystectomy syndrome
- Hernia