Hemorrhoidectomy is the surgical excision of hemorrhoids. Today, this simple excision of the hemorrhoidal mass is most frequently employed to treat hemorrhoids. The history of surgical treatment of hemorrhoids is vast; a detailed account can be found here. Today, the most common method used to treat internal hemorrhoids is closed hemorrhoidectomy, or the Ferguson technique, named after James A. Ferguson who described the technique in 1955.
Indications
- External hemorrhoids with excessive pain or failure to respond to conservative treatment
- Internal hemorrhoids not resolved with rubber band ligation
- Bleeding
- Protrusion
- Pain
- Pruritus
- Infection
Contraindications (general)
- Serious systemic disease (cirrhosis of the liver, etc.)
- Probable short life expectancy
Preoperative Consideration
- Cleaning enema night before/early morning (several hours prior)
Relevant Anatomy
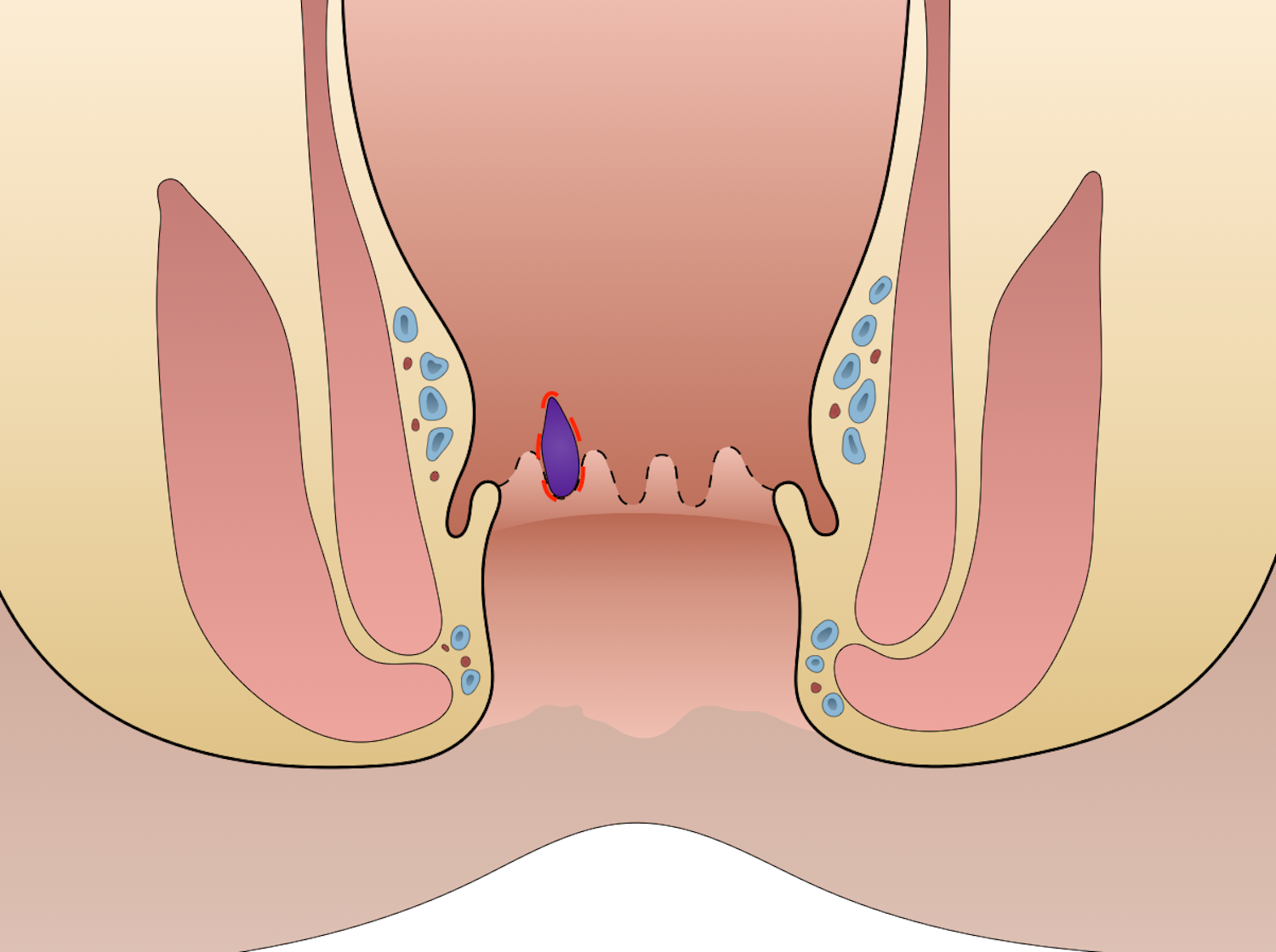
- Anal verge: external boundary of the anal canal
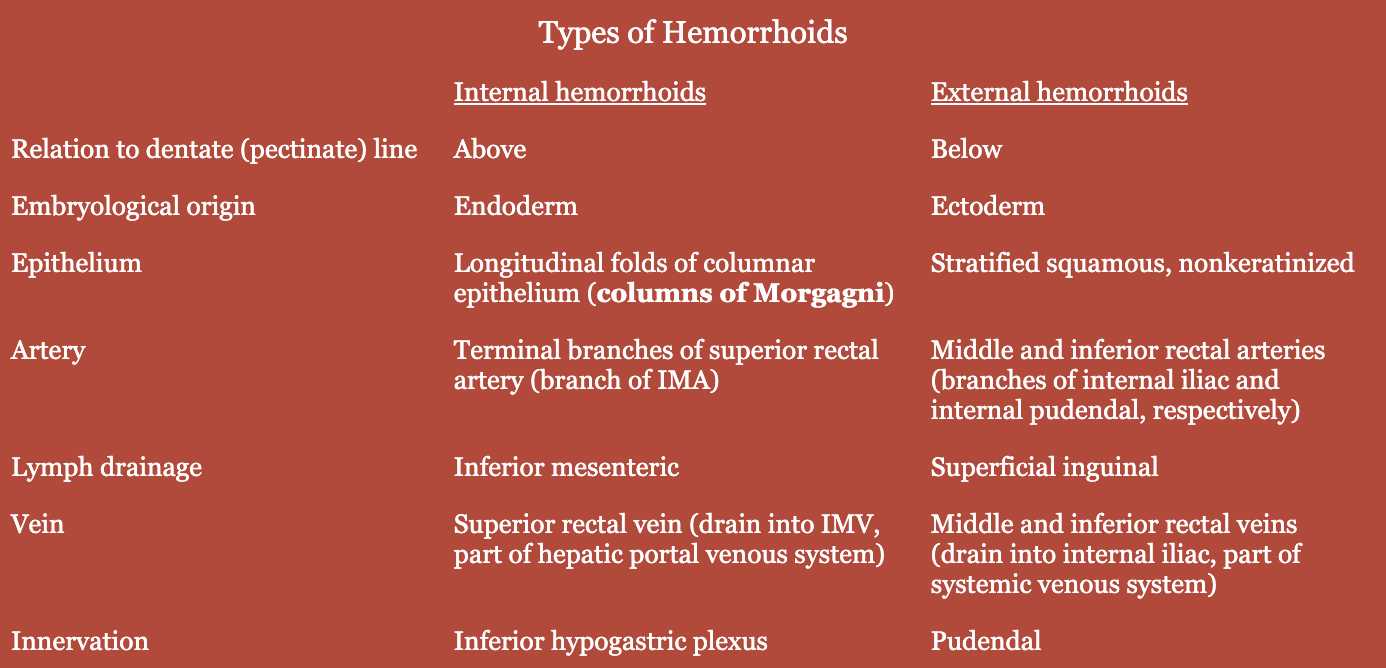
- Pectinate line: [dentate line] divides the upper 2/3 from the lower 1/3 of the anal canal
- Small fibrous bands running into hemorrhoidal tissue are continuation of longitudinal muscle
Relevant Information
- Simple internal hemorrhoids that prolapse may be treated with rubber band ligation
- Dilation of the anus stimulates the respiratory center
- All possible mucosal tissue is preserved in order to prevent anal stenosis
- Degrees of internal hemorrhoids
- First degree: doesn’t prolapse
- Second degree: prolapses but returns on its own
- Third degree: prolapses and requires active manual reduction
- Fourth degree: can’t be reduced
- Three hemorrhoid locations → max number of internal hemorrhoids possible to have is 3
- Left lateral
- Right posterior (most common location for external)
- Right anterior
- Hemorrhoidectomy techniques
- Closed (Ferguson) hemorrhoidectomy: closes mucosa
- Most commonly used technique
- Closes the mucosa with sutures after hemorrhoid tissue removal
- Associated with less postoperative pain, faster healing, and reduced risk of postoperative bleeding compared to open (Milligan-Morgan) hemorrhoidectomy
- Open (Milligan-Morgan) hemorrhoidectomy: leaves mucosa open
- Closed (Ferguson) hemorrhoidectomy: closes mucosa
Surgical Technique
- Patient positioned
- If spinal anesthesia → prone jackknife
- If general anesthesia → exaggerated dorsal lithotomy
- Anoscopy is completed, identifying any associated pathology. Hypertrophies papillae or deep crypts may be removed.
- The anal canal is gently dilated to 2 fingers’ width for adequate exposure. A self-retaining retractor is inserted into the canal and further inspection is made. A gauze sponge is inserted into the rectum and the reactor is withdrawn. The surgeon uses the sponge to create gentle traction in order to reproduce the effect of a passing bolus through the canal. As the sponge is withdrawn, the prolapsing hemorrhoids are visualized and picked up with hemorrhoid clamps. Clamps are placed on all hemorrhoids and left as markers during the operation.
- Opposite the hemorrhoid, a straight hemostatic forceps is placed on the anal verge. The hemorrhoid is placed under tension by simultaneous traction on the forceps and the hemorrhoid clamp. A triangular incision is made from the anal verge to the pectinate line. By using traction on the two clamps, it’s possible to dissect the triangular area of skin and hemorrhoid tissue from the outer ends of the external sphincter muscle. Dissection is carried to the outer edge of the external sphincter. The anal skin must be divided to and slightly beyond the pectinate line.
- Now what remains is mucosa and deep veins entering the hemorrhoid. A straight clamp is placed on the tissue and a transfixing suture is placed at the apex of the hemorrhoidal mass. Then the hemorrhoidal tissue is excised with a scalpel and an over-and-over continuous suture is made in the mucosa. The clamp is removed and a continuous suture is used to approximate the mucosa, including the two edges of the pectinate line. As the suture is continued externally, small bites are taken in the external sphincter muscle. The deep portion of the skin is closed with subcutaneous suture, and skin edges are left open for optimal drainage.
- This process is repeat for all other hemorrhoidal masses.
Postoperative Complications
- Urinary retention (most common)
- Bleeding
- Infection
- Fecal incontinence
- Fecal impaction
- Anal stenosis
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Management of Hemorrhoids,” (2024)