The first attempts of intestinal surgery were done in response to emergency conditions, usually a wound. Abu Al Qasim Al Zahrawi (Albucasis) (936–1013) used ants for intestinal anastomosis and was the first surgeon to sew the intestine with suture derived from an animal’s gut.
Indications
- Small bowel obstruction
- Malignancy
- Non-traumatic perforation
- Traumatic perforation
- Ischemic necrosis
- IBD
Contraindications (relative)
- Active IBD
Preoperative Considerations
- Stomach emptied and gastric content is suctioned out
- Gastric suction is maintained during surgery
- Fluid and electrolyte balance is established according to clinical situation
- Antibiotics are started if gangrene is suspected
Relevant Anatomy
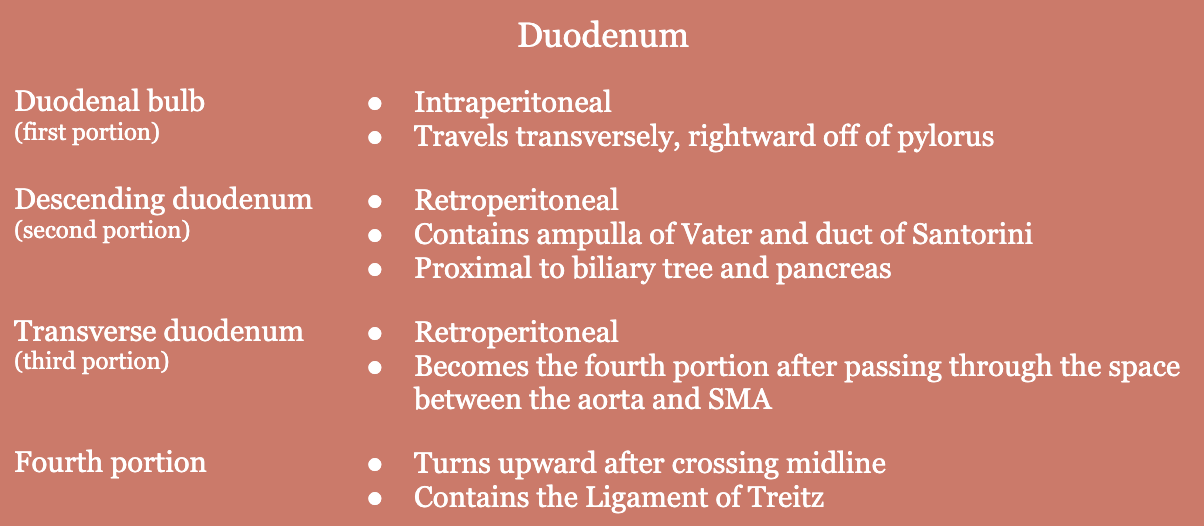
- Small bowel is made up of three section → duodenum, jejunum, ileum
- Iron is primarily absorbed in the duodenum
- Ligament of Treitz: thin muscular band that connects duodenum and jejunum to surrounding connective tissue; serves as marker for transition from the duodenum to the jejunum
- Jejunum
- Site of maximum nutrient absorption (except for B12, bile acids, and folate)
- Blood supply: numerous branches off of the superior mesenteric artery (SMA)
- Ileum
- Absorption site for B12, bile acids, and folate
- Blood supply: numerous branches off of the superior mesenteric artery (SMA)
Relevant Information
- Types of anastomosis
- Side-to-side
- End-to-end
- End-to-side
- Side-to-end
- End-to-end anastomosis restores the natural continuity of the bowel more accurately than side-to-side anastomosis, which is favored when there is a large discrepancy between the sizes of the ends of bowel that need to be anastomosed
- Determining viability of strangulated bowel
- Cadaveric odor
- Presence of bloody fluid (indicates venous thrombosis)
- Lack of peristalsis over involved intestine
- Loss of normal luster/color of serosa
- Absence of arterial pulsation (most important!)
Surgical Technique
- Patient is placed in the supine position and skin is prepped and draped in the usual sterile fashion. An incision is made over the suspected site of the lesion. A lower midline incision is often used, since the lower ileum is frequently involved. A culture of the peritoneal fluid may be taken, noting the amount, color, and consistency. The dilated loops of intestines are retracted to a warm, moist surface and covered with gauze packs soaked in warm saline. When strangulation is present, the surgeon must determine the viability of the intestine. The viability of the involved intestine may improve after the obstruction is relieved and the bowel has been packed with warm, moist gauze for a few minutes.
- Other ways of detecting viability of the intestines:
- Change in the color of the bowel when 100% oxygen is inhaled – infiltration of the mesentery with 1% procaine hydrochloride solution may overcome vascular spasm and bring about arterial pulsations in questionable cases
- IV injection of fluorescein followed by UV lamp illumination
- Handheld Doppler
- Other ways of detecting viability of the intestines:
- In the presence of tumor, the mesentery should be explored for metastatic lymph nodes.
- The intestines should be resected 5 – 10 cm beyond the grossly involved area. The bowel and mesentery are divided, preferably mesentery first. The surgeon must be sure that: clamps aren’t placed too far down toward the base of the mesentery (blood supply to the long segment of the bowel may be divided accidentally), resection extends into the base of the mesentery only to the presence of malignant disease, sizable pulsating vessels are preserved to nourish the bowel adjacent to the point of resection.
- Mesentery should be cleaned off of the bowel at least 1 cm beyond the line of resection to ensure safe application of serosal suture/stapler. Narrow, straight clamps with atraumatic teeth are applied to the intestine obliquely. The bowel is divided on both sides of the lesion, and the retained bowel is covered with warm, moist sponges. The color of the intestine is observed again to ensure blood supply is adequate. If the intestine appears blue or if there is no pulsation in the mesenteric vessels, the intestine is further resected until circulation is adequate.
- After the bowel ends have been prepared for anastomosis and mobilized distally and proximally to prevent tension on the anastomosis site, the anastomosis can begin.
- Anastomosis
- End-to-end anastomosis with suture. Oblique clamps placed earlier are rotated to present the posterior serosal surface for approximation. Enterostomy clamps are placed along the intestine 5 – 8 cm from the crushing clamps to prevent leakage of intestinal contents after the clamps are removed. Silk mattress sutures are taken in the serosa at the mesenteric and antimesenteric borders. A layer of Halstead 3-0 silk sutures is placed in the serosa. The posterior mucosa is then closed by either a continuous lock stitch of absorbable suture or interrupted 4-0 silk. The antimesenteric angle and anterior mucosa are closed by changing to a Connell inverting stitch. The anterior serosal layer is then closed with interrupted Halstead sutures of 3-0 silk. The mesentery is approximated with interrupted 4-0 silk to avoid injuring vessels. Invaginating the bowel against the thumb with the finger verifies anastomosis patency.
- Side-to-side anastomosis with suture.
- Severed ends of the intestine are closed with continuous inversion suture of absorbable suture over the clamp. The wall of the intestine is inverted, and smooth serosa is approximated as the clamp is withdrawn. The suture is pulled just tight enough to control the bleeding and occlude the lumen and is tied at the mesenteric border. The open end of the intestine can be closed with interrupted 3-0 silk sutures. The bowel end is closed with a serosal row of interrupted 3-0 silk mattress sutures that must not include fat or mesentery. To avoid interference with the blood supply, the final suture may pull the edge of the mesentery up to the point of closure but should not invert or include it.
- Straight intestinal non-crushing clamps are applied to the intestine close to the mesenteric border and near the closed ends to avoid a blind segment beyond the anastomosis. The bowel is held in position with Allis, Babcock, or thumb forceps as the clamps are applied. The clamps are placed together and the field is covered with fresh towels. Traction sutures are placed at either angle of the anastomosis. A row of interrupted 3-0 silk sutures is placed in the serosa. The bowel wall is incised with a knife on either side of the suture line. The incision is lengthened with electrocautery until a stoma 2 – 3 fingers wide is achieved. The posterior mucosa is closed with continuous absorbable suture lock stitch or interrupted 4-0 fine silk sutures. The anterior layer of mucosa is closed with a Connell inverting stitch and the anterior serosal layer with interrupted 3-0 silk mattress sutures. The angles can be reinforced with several interrupted 3-0 silks until the closed ends of the intestine are securely anchored to the adjacent bowel. The mesentery is approximated using 3-0 silks placed in such a way to avoid major blood vessels.
- Side-to-side, functional end-to-end anastomosis with stapler.
- Cutting linear stapler is used to approximate two ends of the divided small bowel. After the bowel has been divided with 1 cm of freed mesenteric border, the ends are aligned by placing traction sutures at the mesenteric and antimesenteric borders. The antimesenteric border is approximated and each linear staples fork is inserted and fired once the bowel has been aligned evenly. The cutting knife within the linear stapler is deployed and the suture line is inspected for bleeding, which is controlled with interrupted sutures if needed.
- Traction sutures are placed on the mesenteric border of each segment and another is placed centrally to allow for traction on the end of the suture line on the antimesenteric border. The common lumen can be closed using a non-cutting linear stapler. The excess bowel is excised.
- The remaining opening is closed in a vertical manner, thus approximating the mesenteric borders previously tagged with traction sutures. This creates crossed staples only at the ends, which are inspected for suture reinforcement. The mesentery is approximated with interrupted suture and the anastomosis patency is evaluated.
- Routine closure of the abdominal wall is performed.
Postoperative Considerations
- Fluid balance is maintained with LRs
- Constant decompression with NG tube is continued until normal emptying of the GI tract begins
Postoperative Complications
- Infection
- Anastomotic breakdown
- Anastomotic leak
- Fistulization
- Adhesions
