Suture Characteristics
- Size: diameter of suture material; minimum diameter to hold tissue; denoted numerically (e.g., 5-0 or 00000), as the number of zeros increases the diameter of the suture strand decreases, 5-0 is smaller than 3-0
- Knot tensile strength: force (lbs.) which breaks the suture when knotted; tensile strength of the suture shouldn’t exceed that of the tissue
- Strand number → monofilament vs. multifilament
- Monofilament
- Single strand
- Pros
- Less resistance
- Less likely to harbor organisms
- Tie down easily
- Cons: crushing or crimping may cause weakness, resulting in breakage of suture
- Multifilament
- Several filaments (or strands) twisted or braided together
- Pros
- Greater tensile strength, pliability, and flexibility
- Can be coated to help them pass through tissue easily
- Coated are often good for intestinal procedures
- Monofilament
- Absorbable vs. nonabsorbable
- Absorbable
- Temporarily hold wound edges until healed sufficiently to withstand normal stress. Some are absorbed rapidly an others are treated or chemically structured to lengthen absorption time
- Can be impregnated or coated with agents to improve handling properties
- Can be dyed to increase visibility
- Made from healthy mammals or synthetic polymers
- Subtypes
- Natural absorbable: digested by body enzymes which attack and break down suture
- Synthetic absorbable: water penetrates suture and breaks down polymer chain (hydrolysis); causes less tissue reaction than natural absorbable
- Absorption time may accelerate if patient has fever, infection, or protein deficiency or if suture is placed in a moist or fluid-filled area
- Nonabsorbable
- Suture not digested by body enzymes or hydrolyzed in body tissue
- Indications
- Exterior skin closure: removed after sufficient healing has occurred
- Within body cavity: remain indefinitely
- Patient history of allergic reaction to absorbable suture, keloid tendency, or possible tissue hypertrophy
- Prosthesis attachment (e.g., defibrillators, pacemakers, drug delivery devices)
- Made of single or multiple filament
- Comprised of metal, synthetic, or organic fibers rendered into a strand by spinning, twisting, or braiding
- May be coated/uncoated, uncolored/naturally colored/dyed
- Absorbable
Types of Suture

Absorbable Gut
- Raw material: submucosa of sheep intestine or serosa of beef intestine
- Characteristics
- Made of highly purified collagen, which determines its tensile strength and ability to be absorbed by the body without adverse reaction
- Rate of absorption depends on type of gut used, type and condition of tissue involved, and patient’s general health status
- Can be used in the presence of infection, but may be absorbed more quickly
- Subtypes
- Plain gut
- Rapidly absorbed
- Tensile strength maintained for 7 – 10 days
- Absorption completed within 70 days
- Uses: tissues that require minimal support → ligating superficial blood vessels, suturing subcutaneous fatty tissue
- Color: light tan
- Fast-absorbing gut
- Heat treated to accelerate to accelerate tensile strength loss and absorption; less tensile strength than plain surgical gut of comparable size
- Uses: epidermal suturing, where sutures only required for 5 – 7 days
- Not for internal use
- Color: light tan
- Chromic gut
- Treated with chromium salt solution to resist body enzymes, prolonging absorption time over 90 days
- Minimizes tissue irritation; less reaction than plain gut during early stages of healing
- Tensile strength retained for 10 – 14 days, some measurable strength up to 21 days
- Color: brown
- Plain gut
Synthetic Absorbable
- Uses: abdominal and chest wound closure, ophthalmic surgery
- VICRYL suture
- Copolymer of lactide and glycolide. Lactide has water-repelling qualities, thus leading to slower water penetration and tensile strength loss compared to natural absorbable sutures. Absorption of suture mass is rapid once tensile strength is lost.
- Size 6-0 and larger
- Retain 75% tensile strength after 2 weeks
- Retain 50% tensile strength after 3 weeks
- Not digested by enzymatic activity and thus have less tissue reaction than surgical gut.
- Color: white (undyed) or violet, green (dyed)
- Coated VICRYL suture
- Smooth synthetic absorbable suture that easily passes through tissue with minimal drag and less tendency to incarcerate tissue
- Can be used in the presence of infection
- Retain 75% tensile strength after 2 weeks
- Retain 50% tensile strength after 3 weeks for sizes 6-0 and larger
- Retain 40% tensile strength after 3 weeks for sizes 7-0 and smaller
- Coated VICRYL RAPIDE
- Braided suture made of same copolymer as coated VICRYL suture
- Absorption rate and tensile strength differ from coated VICRYL suture due to use of a polymer material with a lower molecular weight
- Only available undyed
- Fastest-absorbing synthetic suture
- Lower tissue reaction than chromic gut suture
- Used only for superficial soft tissue approximation of skin and mucosa, where only short-term wound support (7 – 10 days) is required. Not to be used in ligation, in ophthalmic, cardiovascular, or neurologic procedures
- Retain 50% tensile strength after 5 days
- All original tensile strength lost by 10 – 14 days. Absorption is complete by 42 days.
- Monocryl suture
- Monofilament with superior pliability for easy handling and tying
- Virtually inert in tissue and absorbs in a predictable manner
- Often used for subcuticular closure and soft tissue approximations and ligations, with exception of neural, cardiovascular, ophthalmic, and microsurgical applications
- Dyed Monocryl
- Retains 60 – 70% tensile strength after 1 week
- Retains 30 – 40% tensile strength after 2 weeks
- All original tensile strength lost by 28 days
- Undyed Monocryl
- Retains 50 – 60% tensile strength after 1 week
- Retains 20 – 30% tensile strength after 2 weeks
- All original tensile strength lost by 21 days
- Absorption is complete by 91 – 119 days
- Color: natural (undyed) or violet (dyed)
- PDS (polydioxanone) suture
- Monofilament suture which combines features of soft, pliable, monofilament with absorbability and extended wound support for up to 6 weeks
- Elicits slight tissue reaction
- Low affinity for microorganism
- Absorbed in vivo by hydrolysis
- Retains 70% tensile strength after 2 weeks
- Retains 50% tensile strength after 4 weeks
- Retains 25% tensile strength after 6 weeks
- Color: clear (undyed) or violet (dyed)
- Panacryl suture
- Braided synthetic absorbable suture
- Provides extended wound support found in nonabsorbable suture
- Retains 80% tensile strength after 3 months
- Retains 60% tensile strength after 6 months
- Absorption is complete by 1.5 – 2.5 years
- Well-suited in patients with compromised wound healing
- Color: undyed
Nonabsorbable
- Surgical silk
- Represents standard of performance by which newer synthetic materials are judged
- Can be twisted or braided
- Loses tensile strength when exposed to moisture
- Although classified as nonabsorbable suture, long-term in vivo studies show it loses most or all tensile strength in about 1 year and is usually undetectable in tissue after 2 years.
- Surgical stainless steel
- Absence of toxic elements, flexibility, and fine wire size
- Both monofilament and twisted multifilament
- High in tensile strength, low in tissue reactivity, holds a knot well
- Nylon suture
- Derived by chemical synthesis
- Well-suited for retention and skin closure due to elasticity
- Color: clear (undyed) or green, black (dyed)
- NURULON nylon suture
- Braided into multifilament strand
- Handle like silk but have more strength and less tissue reaction than silk
- Loses 15 – 20% tensile strength per year by hydrolyzation
- Color: white (undyed) or black (dyed)
- Mersiline polyester fiber suture
- First synthetic braided suture shown to last indefinitely in the body
- Provide precise, consistent suture tension
- Minimize breakage and virtually eliminate the need to remove irritating suture fragments postoperatively
- EXCEL polyester suture
- Coating eases passage of braided strands through tissue and provides pliability, handling, and smooth tie-down of each knot
- Minimal tissue reaction
- Retain strength in vivo for extended periods
- Primarily used in cardiovascular surgery for vessel anastomosis and placement of prosthetic materials
- Available attached to TFE polymer felt pledgets. Pledgets serve to prevent possible tearing of adjacent friable tissue and are used routinely in valve replacement procedures (to prevent the annulus from tearing when the prosthetic valve is seated and sutures are tied) and in situations where extreme deformity, distortion, or tissue destruction at the annulus has occurred.
- PROLENE polypropylene suture
- Used when minimal suture reaction is desired: contaminated or infected wounds to minimize later sinus formation and suture extrusion
- Color: clear (undyed) or blue (dyed)
- PRONOVA poly suture
- Monofilament nonabsorbable that resists involvement in infection; successfully employed in contaminated and infected wounds to eliminate or minimize later sinus formation an suture extrusion
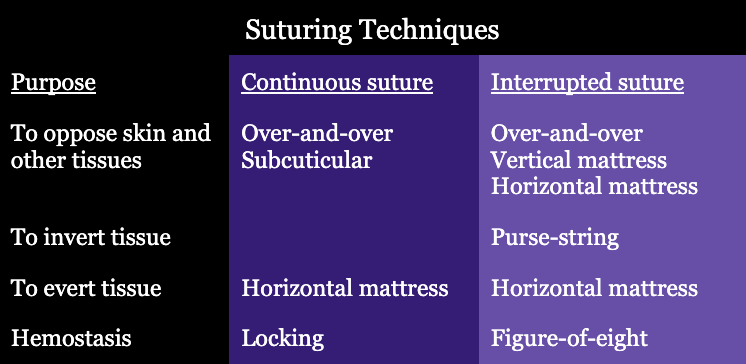
Suturing Techniques
- Ligatures
- Ligature (tie) is a suture tied around a vessel to occlude the lumen
- Free tie OR freehand ligatures
- Stick tie OR suture ligature OR transfixion suture
- Continuous (running) sutures
- Leaves less foreign body in the wound
- Types
- Running locked
- Over-and-over
- Interrupted sutures
- Uses a number of strands to close the wound. Each strand is tied and cut.
- Provides a more secure closure – if one strand breaks, the other strands remain intact.
- Types
- Simple interrupted
- Interrupted vertical mattress
- Interrupted horizontal mattress
- Deep sutures
- Placed completely under the epidermal skin layer
- Placed in a continuous or interrupted fashion
- Not removed postoperatively
- Buried sutures
- Placed so the knot protrudes to the inside, under the layer being closed
- May be useful in thin patients who may be able to feel large knots that aren’t buried
- Purse-string sutures
- Continuous sutures placed around a lumen and tightened to invert the opening
- Uses: in bowel to secure an stapling device, or in an organ prior to insertion of a tube
- Subcuticular sutures
- Placed in dermis, beneath the epithelial layer; in a line parallel to the wound
- Placed in a continuous or interrupted fashion
Knot Tying
One-handed knots
- Know how to throw one-hand knots with your right and left hands
- Video
- How to practice
- You can place suture material most places (e.g., water bottle, backpack, steering wheel, etc.) and practice throughout the day on your rotation and also in your spare time.
- Suture material: it may be easier to start with larger cords and progressively get closer to suture size
- Cord: this can be purchased online and can have different colors that may help visualize the structure of your knots, but climbing cord is often cheaper (and re-usable)
- Twine, string, or yarn: easy to buy in bulk, still very easy to see knots (don’t buy black!), and a little bit smaller in size to begin the transition to smaller material
- Thread: a cheap, easy alternative to actual suture
- Suture: ask scrub techs for expired/unused throws and sutures to practice with
Two-handed knots
- Video
- How to practice: same as one-handed knots
Deep tie
- Made in the recesses of the body cavity or hard-to-reach areas
- How to practice: place a small command hook inside a small plastic cup and practice pushing your knot past the hook to simulate the difficulty of throwing knots into a deep hard-to-reach space
Instrument tie
- Basic, simple, effective way to tie knots, but takes longer than hand ties
- Helpful to utilize when running low on suture or when trying to conserve suture length
- Video
- How to practice: use suture kit and follow video using suture pad
Ligation around a hemostat
- Used to ligate a clamped vessel or piece of tissue
- With an assistant holding the tips of the hemostat up, a free tie is placed under the hemostat and a knot is thrown to occlude the lumen of the vessel. The assistant may flash or slowly release the clamp depending on the scenario, at the surgeon’s direction. With the clamp removed, the knot is tightened further prior to throwing additional knots.
- Video
- How to practice: have a friend hold a hemostat to practice maneuvering around a hemostat, then practice knots on your own to build knot tying skill
Endoscopic knot tying
- Extracorporeal knot tying (through a trocar)
- Suture penetrates tissue and both needle and suture are removed from the body cavity through the trocar
- Series of half-hitches are tied, each one being pushed down into cavity and tightened with endoscopic knot pusher
- Intracorporeal knot tying (directly within the abdominal cavity)
- After suture penetrates tissue, the needle is cut and removed
- Several loops are made with the suture around the needleholder and the end of the suture is pulled through the loops
- Steps are repeated to form a surgeon’s knot, which is tightened with a knot pusher
- Video
- How to practice: utilize laparoscopic trainer at your residency program, buy one online, or ask if product reps will work with you as a resident to obtain one
Surgical Needle
Elements
- Strength: how the needle resists deformation during repeated passes through tissue
- Ductility: the needle’s resistance to breaking under a certain amount of pressure
- Sharpness: related to the angle of the point as well as the taper ratio of the needle; tapered needles usually have a ratio of 8:1, 12:1, etc.
- Stability: how stable the needle is in the needleholder; most needles are flattened at the grasping area to increase needle control
Needle Characteristics
- Needle Anatomy
- Chord length: straight line distance between the point of the curved needle to the swage
- Needle length: curved distance along the needle from point to end
- Radius: distance from the center of the circled needle to the body of the needle if the curvature of the needle were continued to make a full circle
- Diameter: gauge/thickness of the needle wire
- Eye
- Closed (Mayo): eye, similar to household sewing needle where suture can be threaded through the eye and needle can be reused with different suture
- French (split or spring): slit from inside the eye to the end of the needle with ridges that catch and hold the suture in place
- Swaged (eyeless): suture is firmly attached to the needle
- Popoff: suture is loosely attached to the needle
- Body: portion of the needle grasped by the needle holder
- Needle point: extends from the extreme tip of the needle to the maximum cross-section of the body
- Needle shapes
- Straight needle: used when suturing tissues that are easily accessible
- Keith needle: straight cutting needle, used for abdominal wounds (e.g., Cesarean section)
- Bunnell needle: used for tendon repair
- Half-curved needle (“ski” needle): used for skin closure or in laparoscopy
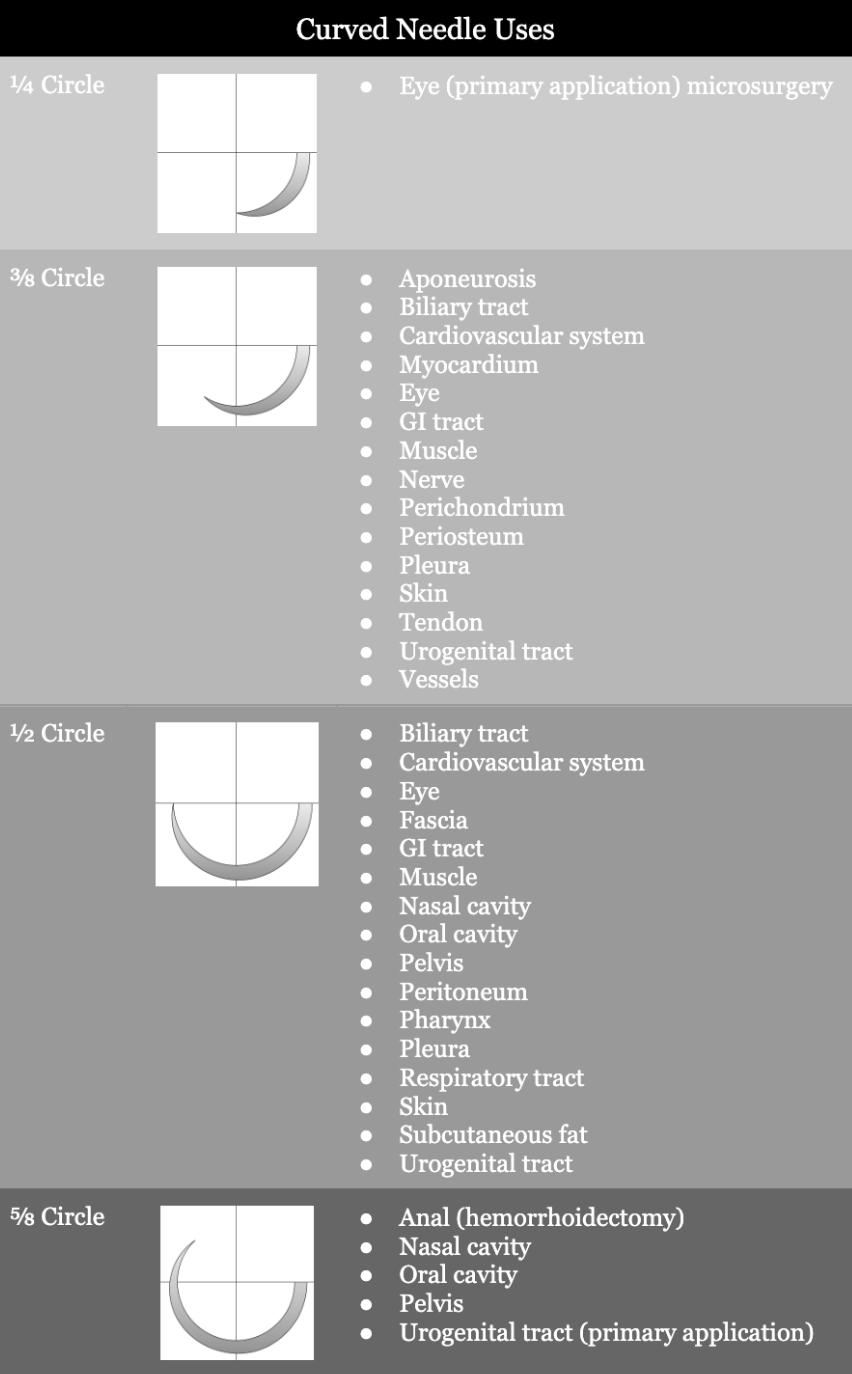
- Curved needle
- Used most often
- Shape requires less space for maneuvering than a straight needle
- Curvature may be ¼, ⅜, ½, or ⅝
- Straight needle: used when suturing tissues that are easily accessible
- Compound curved needle: initial curvature allows for reproducible, short, deep bites into the tissue; the remaining portion of the body forces the needle out of the tissue and permits a view into the wound to ensure equidistance of suture material on both sides of the suture
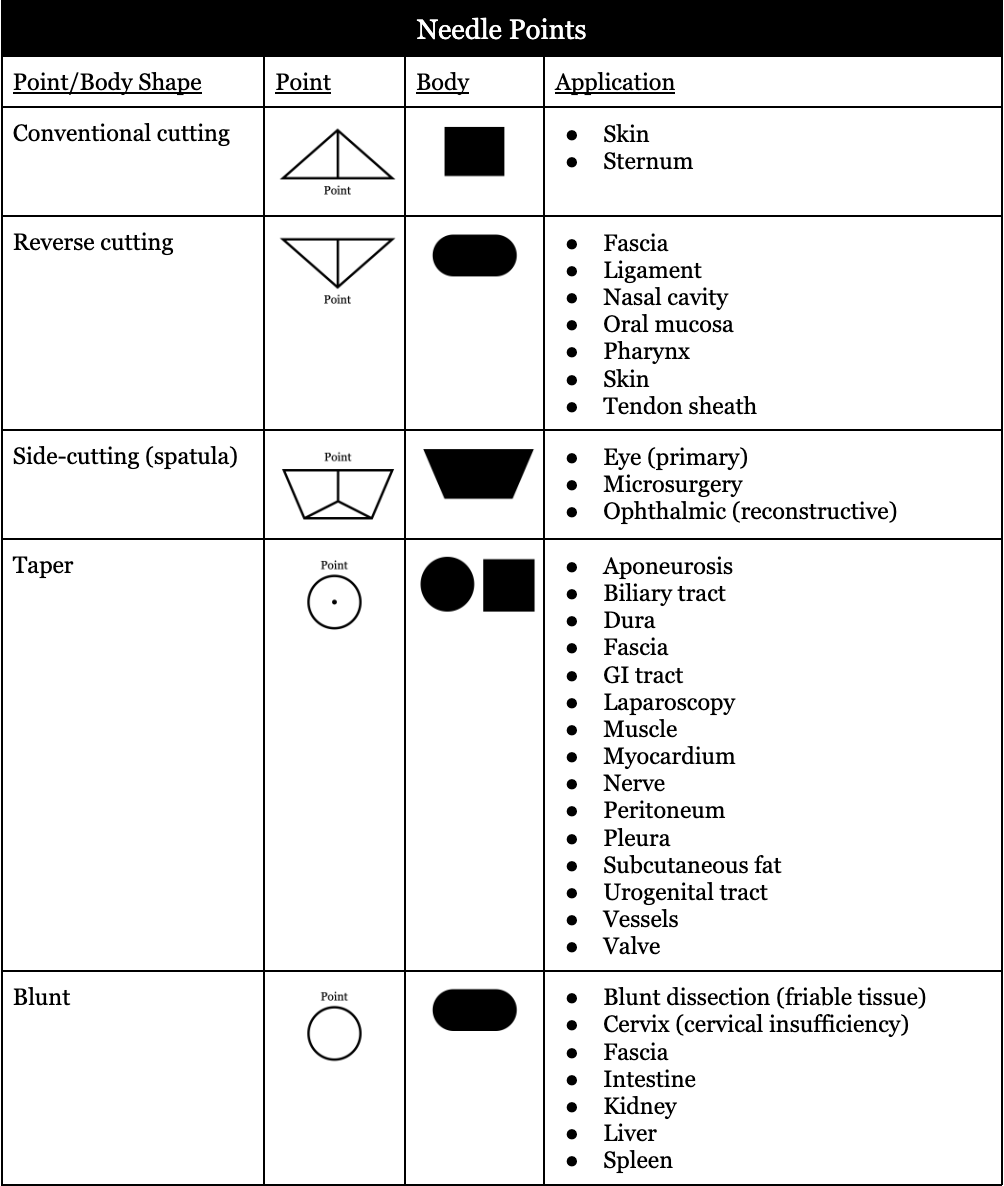
- Needle points
- Cutting needles: have at least two opposing cutting edges; sharpened to cut through tough tissue that is difficult to penetrate
- Conventional cutting needles: in addition to two cutting edges, there is a third cutting edge on the inside concave curvature of the needle
- Reverse cutting needles: in addition to two cutting edges there is a third cutting edge on the outer convex curvature of the needle; more strength than similar-sized conventional cutting needle, danger of tissue cutout is decreased, hole left by the needle leaves a wide wall of tissue against which the suture can be tied
- Side-cutting needles (spatula needles): flat on top and bottom; allow the needle to separate/split through thin layers of sclera or corneal tissue and travel within the plane between them
- Taper point needles (round needles): pierce and spread tissue without cutting it; needle body flattens to an oval or rectangular shape
- Blunt point needles: can dissect friable tissue rather than cutting it; have a taper body with a rounded, blunt point that will not cut through tissue
- Cutting needles: have at least two opposing cutting edges; sharpened to cut through tough tissue that is difficult to penetrate