Colonic pseudo-obstruction (Ogilvie syndrome) occurs when there is acute dilation of the colon with no mechanical obstruction. It was first described in 1948 by the British surgeon William Heneage Ogilvie.
Epidemiology
- Usually in elderly and comorbid patients
- Classically follows acute illness; see table with association conditions below
Pathogenesis
- Several proposed theories
- Autonomic imbalance; excess sympathetic activity
- Disrupted colonic reflex arcs
- Chronic disease
- Medications
Physical Exam
- Abdominal distention
- Abdominal pain
- Nausea
- Vomiting
- Obstipation
- Diarrhea
Labs
- BMP: low K, Mg, Ca
Imaging
- Abdominal X-ray → distended colon, with largest diameter usually at cecum and right colon (up to 10 – 12 cm in diameter), dilation and gas continuing to distal rectum; no evidence of mechanical obstruction
- Water-soluble contrast enema
- Distinguish between mechanical obstruction and pseudo-obstruction
- Abdominal CT
- Typically used as confirmatory test
- Distinguishes obstruction type and assesses for ischemia and impending perforation
- Endoscopy is not recommended for diagnostic purposes due to risk of perforation.
Treatment
- Stepwise approach depending on degree of distention, perforation risk, and patient response
- Supportive care
- NPO
- Electrolyte disturbance correction
- Fluid resuscitation
- Encourage ambulation, prone positioning, and knee-chest position to help with passing flatus
- Discontinue medications associated with pseudo-obstruction
- NG tube and rectal tube insertion may help
- Monitor patient response with serial physical exams and daily abdominal X-rays
- Indications: patients with cecal diameter < 12 cm without evidence of ischemia or perforation
- Avoid: osmotic and stimulant laxatives as they can worsen colonic dilation
- Colonic decompression is indicated in patients that do not improve with supportive care
- Pharmacologic decompression treatment → neostigmine
- MOA: acetylcholinesterase inhibitor (parasympathomimetic); stimulate muscarinic receptors to enhance colonic motor activity and stimulate peristalsis leading to flatus and bowel movements
- 2 – 2.5 mg IV bolus over 3 – 5 minutes
- Indications: patients unresponsive to supportive treatment
- Contraindications: mechanical bowel obstruction, patients significant cardiac disease, asthma, or signs of ischemia or perforation
- Side effects: vomiting, crampy abdominal pain, sialorrhea, bradycardia
- Endoscopic decompression → colonoscopy
- Goal is passage of scope to right colon with minimal insufflation and narcotic use, place colonic decompression tube while removing as much gas from the colon as possible
- Indications: patients with contraindications to neostigmine, patients unresponsive to neostigmine
- Surgery
- Surgical technique varies depending on the clinical situation. Patients who are complicated by colonic ischemia or perforation or those who have failed other treatments usually undergo surgery with stoma creation (decompressing loop colostomy) with or without resection.
- Indications: patients who do not respond to other lines of treatment, patients with signs of systemic toxicity, ischemia, or perforation
Relevant Information
- Signs of ischemia and impending perforation
- Abdominal tenderness
- Leukocytosis
- Fever
- Cecal dilation > 12 cm
- Colonic ischemia or perforation occurs in 3 – 10% of patients and is more common in patients with cecal diameter > 12 cm and/or dilation duration > 6 days

- Large bowel = colon + rectum; 150 cm in length (roughly 5 feet)
- Covered with peritoneum; no mesentery
- Cecum
- Thinner wall and larger diameter compared to the rest of the colon
- Most likely location to perforate in presence of large bowel obstruction
- Risk of ischemic necrosis and perforation increases with diameter > 12 cm
- Ileocecal valve
- Where terminal ileum empties into cecum
- Thickened, nipple-shaped invagination containing circular muscle
- Appendix
- Extends from cecum 3 cm below ileocecal valve
- Blind-ending elongated tube 8 – 10 cm in length
- Ascending colon
- Begins at ileocecal junction and continues to hepatic flexure
- 15 cm in length (0.5 feet)
- Covered with peritoneum anteriorly and laterally
- Fixed against retroperitoneum by fascia of Toldt posteriorly
- Best mobilized along lateral peritoneal reflection by incising “white line of Toldt”
- Transverse colon
- 45 cm in length (roughly 1.5 feet)
- Covered by visceral peritoneum
- Greater omentum is attached at superior aspect; lifting upward with downward traction will reveal an avascular plane adjacent to the colon (most easily identified close to midline)
- Descending colon
- Begins at splenic flexure (where intestine loses its mesentery) to the sigmoid colon
- Splenic flexure
- Where transverse colon is flexed downward
- Suspended by four mainly avascular ligaments
- Phrenicocolic ligament
- Splenocolic ligament
- Renocolic ligament
- Pancreaticocolic ligament
- Sigmoid colon
- Begins at or below level of iliac crest where colon becomes completely intraperitoneal again
- Thicker and more mobile compared to descending colon
- When mobilizing, the mesenteric fold is the surgical landmark for underlying left ureter
- Ends at rectosigmoid junction (where colonic taenia confluence for form complete longitudinal muscle layer, and colon loses its mesentery)
- Splenic flexure
- 25 cm in length (0.82 feet)
- Commonly dissected along the line of Toldt from below and then enter lesser sac by lifting omentum above transverse colon
- Lesser sac (lesser peritoneal sac, omental bursa)
- Potential space that exists within the abdomen between the stomach and the pancreas
- Formed by greater and lesser omentum
- Lesser sac (lesser peritoneal sac, omental bursa)
- Smaller in diameter than ascending colon
- Begins at splenic flexure (where intestine loses its mesentery) to the sigmoid colon
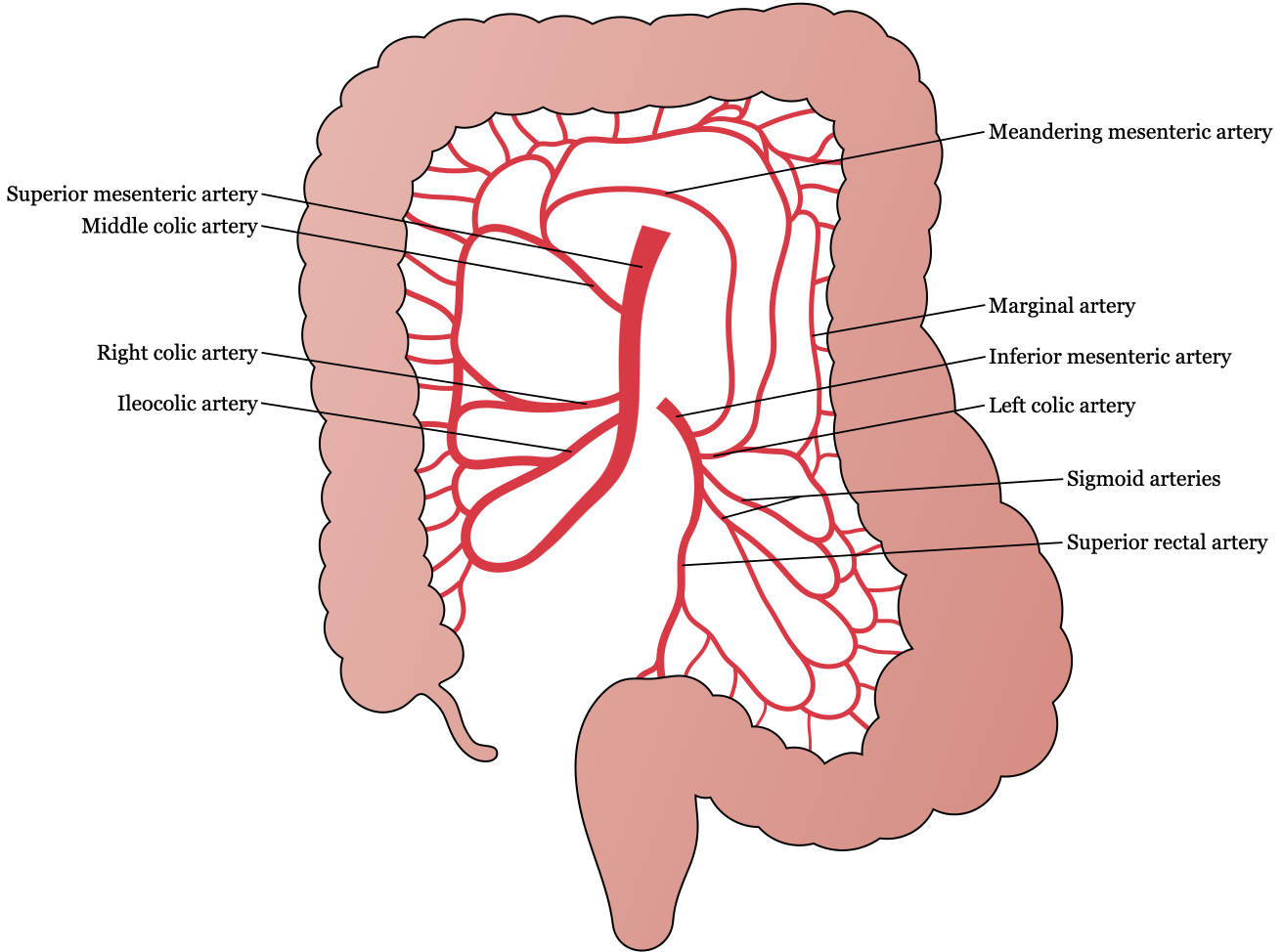
- Meandering mesenteric artery (arc of Riolan, Moskowitz artery)
- Thick collateral vessel that courses closely to the base of the mesentery
- Connects SMA or middle colic artery to the IMA or left colic artery
- Presence suggests occlusion of one of the major mesenteric arteries
Differential Diagnoses
- Mechanical obstruction
- Toxic megacolon due to C. difficile
- Toxic megacolon due to other causes
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Management of Colonic Volvulus and Acute Colonic Pseudo-Obstruction,” (2021)