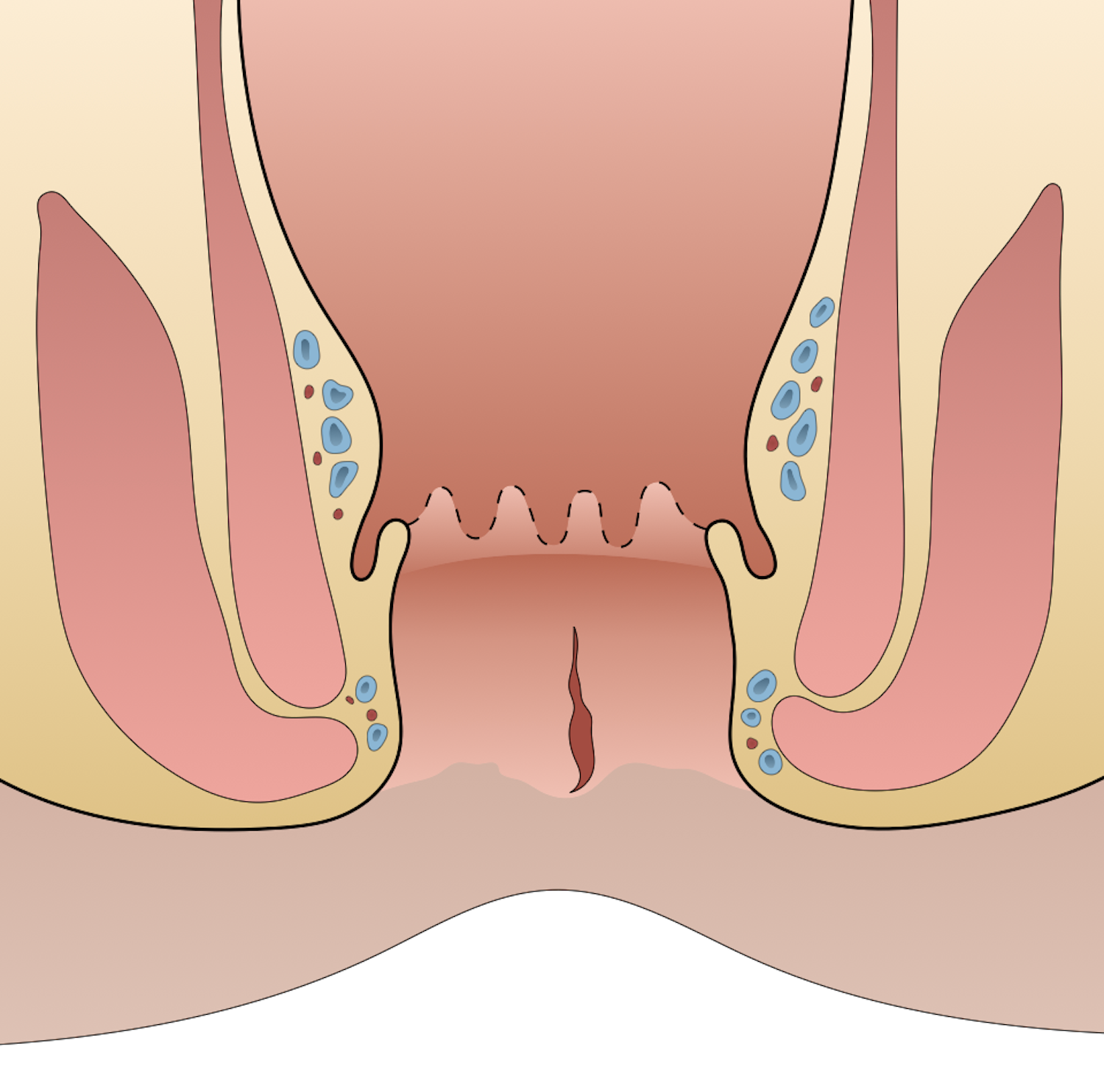
Anal fissures occur when there is a tear in the anal canal that usually extends from the dentate line to the anal verge. The most effective treatment for anal fissures, lateral internal sphincterotomy, was first completed by Stephen Eisenhammer in 1951.
Etiology
- Hard stool
- Explosive diarrhea
- Anal receptive intercourse
- Anal trauma
- Surgical instrumentation
Pathogenesis
- Multiple proposed mechanisms
- Most anal fissures occur at posterior midline
- Area of greatest stress
- Relative ischemia of the area
History
- Symptoms are often cyclical
- Sharp anal pain with defecation, “passing pieces of glass/razor blades”
- Anal pain followed by throbbing and anal spasm
- Anal bleeding
- Acute fissure
- Present < 6 weeks
- Bright red bleeding with bowel movements
- Sharp, burning, tearing anal pain/spasm that can last for hours after bowel movement
- Chronic fissure
- Present for > 6 – 8 weeks
- Pain with defecation is less severe than with acute fissure
Physical Exam
- Visual inspection of anus reveals fissure → linear separation of anotherm
- If fissure is not visible, gentle pressure with cotton tip on posterior and anterior aspect of the anal canal can reproduce the exam
- Exam under anesthesia if diagnosis is unclear
- Acute fissure: longitudinal line
- Chronic fissure: exposed internal sphincter fibers at the base, hypertrophied anal papilla proximally, and skin tag or sentinel pile (i.e., thickened mucosa/skin at the distal end of an anal fissure often confused with a small hemorrhoid) distally
- Atypical fissures
- Occur anywhere in anal canal
- Tend to be associated with other conditions (e.g., malignancy, Crohn disease, HIV, syphilis, tuberculosis)
Treatment
- Treatment goals
- Address etiology (e.g., constipation, anal trauma cause)
- Relax and dilate internal anal sphincter to improve blood flow and for allow healing
- Address pain and bleeding symptoms
- Medical management
- Majority of acute anal fissures resolve with medical management. Chronic fissures are less likely to heal with conservative measures
- Increase fluid and fiber ingestion
- Sitz baths ± mineral oil or stool softener
- Topical application of nitrates and calcium channel blockers (CCBS)
- Leads to sphincter relaxation, vasodilation, improved blood flow
- Nitrates
- 0.1%, 0.2%, or 0.4% glyceryl trinitrate ointment
- Side effects: headache (occurs in 30% of treated patients)
- CCBs (e.g., diltiazem, nifedipine)
- Similar efficacy to nitrates
- Better side effect profile than nitrates
- Topical treatment preferred over oral treatment
- Botulinum toxin
- Similar results compared to topical therapies
- MOA: inhibit ACh at neuromuscular junction
- Temporary paralysis of the anal sphincter
- 20 – 100 IU will usually result in relaxation of the anal sphincter for 3 months
- Side effects: increased urinary residual volume, heart block, skin irritation, allergic reactions
- Lateral internal sphincterotomy (LIS)
- Most effective therapy to heal anal fissures
- Sustained partial relaxation of internal anal sphincter, resulting in decreased anal sphincter tone
- Can be offered first-line for patients with chronic anal fissures and no fecal incontinence. Excluded as first-line treatment in patients with prior obstetric injuries, IBD, previous anorectal operations, and documented anal sphincter injury.
- Procedure → no significant difference in outcomes between open and closed sphincterotomies
- Radial incision in anoderm that exposes internal sphincter muscle
- Distal segment of internal anal sphincter divided for length of anal fissure
- Wound left open or primarily closure
- Closed LIS: insert narrow-bladed scalpel directly into intersphincteric groove and divide internal sphincter lateral to medial toward surgeon’s finger within anal canal
- Superior to topical nitrates, calcium channel blockers, or botulinum toxin
- Complications: fecal incontinence (8 – 30%, usually self-resolves in 30 days)
- Contraindications: Crohn disease, ulcerative colitis, women of childbearing age, prior obstetrical injury, history of incontinence, sphincter dysfunction
Relevant Information
- Anal fissure locations
- Posterior midline (73%) → most common location
- Anterior midline
- Second most common location
- More common in women
- Atypical fissure: lateral fissure or multiple fissures
- Requires more comprehensive evaluation due to association with other diagnoses
- Differential diagnosis
- Crohn disease
- Anal cancer
- Tuberculosis
- HIV
- Syphilis
- Herpes
- Leukemia
- Dentate line
- Lies midpoint in the anal canal
- Proximal: longitudinal folds of columnar epithelium (columns of Morgagni)
- Distal: smooth squamous epithelium (anoderm)
- Anal verge: where anal canal connects to the outside skin at the anus

Complications
- Bleeding
- Pain
- Infection
- Incontinence
- Fistula formation
Differential Diagnoses
- Hemorrhoids, external
- Perianal abscess
- Sexually transmitted infections
- IBD
- Tuberculosis
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Management of Anal Fissures,” (2022)