Diverticulitis occurs when there is inflammation of diverticula, the abnormal outpouchings of the colonic wall. Graser first described diverticulitis in 1899. Left-sided diverticulitis is most common in the Western world and is the focus of this page.
Etiology
- Risk factors: Western diets high in red meat, fat, and refined grains, central obesity, smoking
- Protective factors: increased fiber intake, physical activity
Epidemiology
- Diverticulitis occurs in a small percentage of people with diverticulosis
Pathogenesis
- Obstruction of the orifice of a diverticulum, leading to stasis, bacterial overgrowth, inflammation, and increased pressure causing ischemia and microperforation
History
- Anorexia
- Nausea
- Urinary urgency (if bladder is secondarily inflamed)
Physical exam
- Fever
- Vomiting
- LLQ abdominal pain with localized tenderness
- Abdominal distention
- Change in bowel habits → diarrhea (35%) or constipation (50%)
- Rectal bleeding is rare → consider IBD or ischemic colitis if present
Labs
- Leukocytosis
- Elevated ESR
- Elevated CRP: may be indicative of complicated diverticulitis
- Procalcitonin
- Fecal calprotectin: maybe associated with diverticulitis recurrence
Imaging
- Flat and upright plain films
- Diagnose obstruction or free intraperitoneal air
- Nonspecific
- CT abdomen and pelvis with water-soluble PO or rectal contrast and IV contrast
- Best initial imaging for suspected diverticulitis (even without contrast)
- Best for confirming diagnosis, excluding others, and classifying severity
- Can stratify patients according to Hinchey classification
- Findings: diverticula, colonic wall thickening, pericolic fat stranding, abscess formation
- US, and MRI can be used for initial evaluation of suspected acute diverticulitis if CT is unavailable or contraindicated
- Flexible endoscopy during acute diverticulitis should be used with caution, as perforation is a risk.
Treatment
- Inpatient management
- If patient is unable to tolerate oral intake, excessively vomiting, showing signs of peritonitis, immunocompromised, at an advanced age
- IV antibiotics (Gram-negative rods and anaerobes for 3-5 days) before switching to PO antibiotics (for 10-14 days)
- Antibiotics are appropriate for high-risk patients with significant comorbid conditions, signs of systemic infection, or immunocompromised status
- Nonoperative treatment of diverticulitis may include antibiotics
- Select patients with uncomplicated diverticulitis can be treated without antibiotics
- IVF
- Pain management
- Bowel rest
- Goal: defervescence and improvement in leukocytosis for 2-4 days. If not, alternative diagnoses or complications should be suspected. Surgical evaluation should be considered.
- Surgery → Hartmann procedure (usually)
- Surgical options
- Hartmann procedure (traditional mainstay surgery): resection of involved colonic segment with colostomy creation, shorter surgery
- Colon resection with primary anastomosis and diverting ileostomy: higher rate of ostomy reversal compared to Hartmann
- Reserved for significant complications, if there is an inability to exclude malignancy, or in those who fail nonoperative treatment
- Restoring bowel continuity after resection should incorporate patient factors, intraoperative factors, and surgeon preference
- Surgical options
- Outpatient management
- Bowel rest
- Increased fluid intake
- PO antibiotics (single or multiple drug regimen for Gram-negative rods and anaerobics), usually quinolones or sulfa drugs + metronidazole OR single agent amoxicillin-clavulanate → systematic review and metaanalysis assessing antibiotics in cases of uncomplicated diverticulosis haven’t shown an accelerated recovery rate, prevention of complications, or later surgery
- Abscesses
- Abscesses >3 cm: image-guided percutaneous drainage in stable patients
- Abscesses <3 cm
- Antibiotics alone
- Can be outpatient if patient is stable
- If antibiotics alone fail, percutaneous drainage is considered
- Antibiotics plus percutaneous drainage
- Antibiotics alone
- Elective surgery
- Elective colonic resection is considered after successful nonoperative treatment of diverticular abscess because the recurrence rate of diverticulitis is substantial, especially with history of diverticular abscess.
- Elective colectomy is typically recommended for patients with diverticulitis complicated by fistula, obstruction, or stricture.
- Elective sigmoid colectomy should be individualized in patients who have recovered from uncomplicated acute diverticulitis.
- Distal anastomosis is (ideally) made to the upper rectum. Rectum is usually not affected by diverticulitis, as it has an additional layer of muscle not found in the colon.
- Follow-up colonoscopy is recommended 4-8 weeks after resolution of symptoms in order to rule out malignancy and inflammatory bowel disease, if it was not performed recently.
- Data suggesting follow up be conducted at 6 weeks is weak
- CT findings suggesting occult malignancy: abscess, shouldering (leading edges of mass have a shelf-like appearance), obstruction, mesenteric or retroperitoneal lymphadenopathy
Relevant Information
- Nuts, seeds, and popcorn are NOT associated with increased risk of diverticulosis, diverticulitis, or diverticular bleeding
- Diverticula
- Saccular outpouchings of the bowel wall
- True diverticula
- Contain all layers of the bowel wall
- Rare, usually congenital
- False diverticula
- Contain only mucosa and muscularis mucosa layers of the bowel wall
- Common incidental finding on routine colonoscopy
- Right-sided diverticulitis is common in Asian countries. It usually affects younger patients and can be difficult to differentiate from acute appendicitis, among other diagnoses
- In elective surgery for diverticulitis, the distal anastomosis is (ideally) made to the upper rectum. Rectum is usually not affected by diverticulitis, as it has an additional layer of muscle not found in the colon.
Complications
- Abscess formation → most common complication
- Fistula (colovesicular fistula is most common)
- Partial bowel obstruction or pseudo-obstruction
- Peritonitis
- Sepsis
Classification System
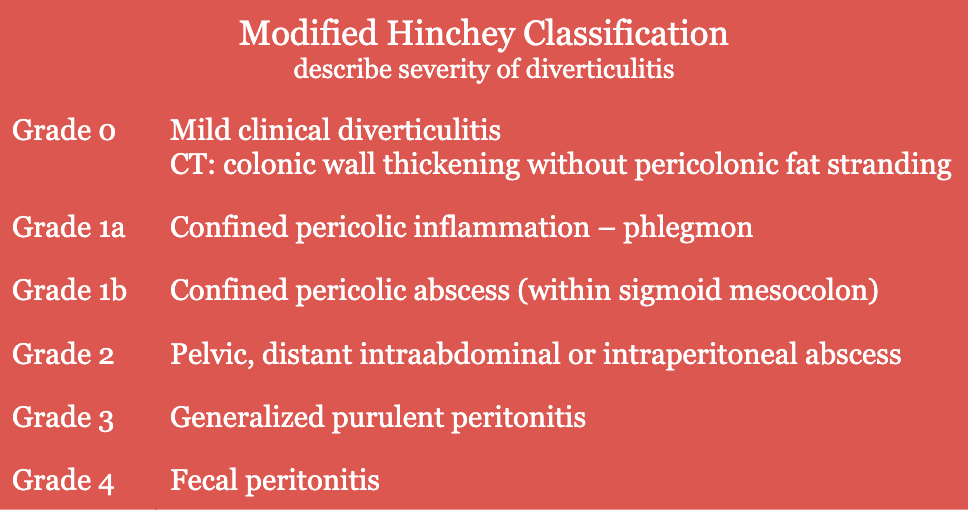
- CT scan has a limited ability to distinguish between Grade 3 and Grade 4 → accurate diagnosis is made in the OR
Differential Diagnoses
- Ischemic colitis
- Inflammatory bowel disease
- Chronic mesenteric ischemia
- Constipation
- Colovesicular fistula
- Intestinal perforation
- Irritable bowel syndrome
- Large bowel obstruction
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis,” (2020)