Ventral hernias are hernias that occur through the anterior abdominal wall.
Etiology
- No conclusive evidence showing that the type of suture used at the primary operation is linked to hernia formation.
- Some data suggests the technique used to close a midline laparotomy is associated with incisional hernia formation → STITCH trial
- Risk factors: obesity, male, sleep apnea, emphysema, prostatism
- Types
- Umbilical hernias
- Children
- Umbilical hernias in infants are common; usually congenital
- Usually close spontaneously by 2 years old
- Treated surgically if they persist past 5 years old
- Adults
- Usually acquired
- More common in women and in patients with conditions that increase intraabdominal pressure
- Risk factors: pregnancy, obesity, ascites, chronic abdominal distention
- Treatment
- Small, asymptomatic umbilical hernias don’t need surgical repair
- Surgical repair considered in patients with
- Large hernia
- Incarceration
- Thinning of overlying skin
- Uncontrollable ascites
- Surgical repair approach
- Defects < 3 cm are often closed primarily
- Defects > 3 cm are often closed with mesh
- Children
- Epigastric hernias
- Occur from the xiphoid process to the umbilicus
- 2 – 3 times more likely in males
- Small defects; often produce pain out of proportion to their size due to incarceration of preperitoneal fat
- Treatment
- Surgical repair (excision of incarcerated preperitoneal tissue and closure of fascial defect)
- Incisional hernias
- Result from excessive tension and inadequate healing of a previous incision; may be associated with surgical site infection
- Risk factors: obesity, advanced age, malnutrition, ascites, pregnancy, conditions that increase intraabdominal pressure, chronic pulmonary disease, diabetes mellitus
- Presentation: enlarge over time, abdominal pain, bowel obstruction, incarceration, strangulation
- Treatment
- Defect ≤ 2 – 3 cm in diameter: primary repair
- Defect resulting from technical error at initial operation: primary repair
- Defects > 2 – 3 cm in diameter: repaired with prosthesis due to high recurrence rate if closed primarily
- Umbilical hernias
Physical exam
- Patient examined in standing and supine position – Valsalva is helpful to demonstrate size and site of hernia
Imaging
- Can be useful adjuncts in cases of unusual hernias
- CT
- DASH (dynamic abdominal sonography for hernia) performed by surgeon
Relevant Information
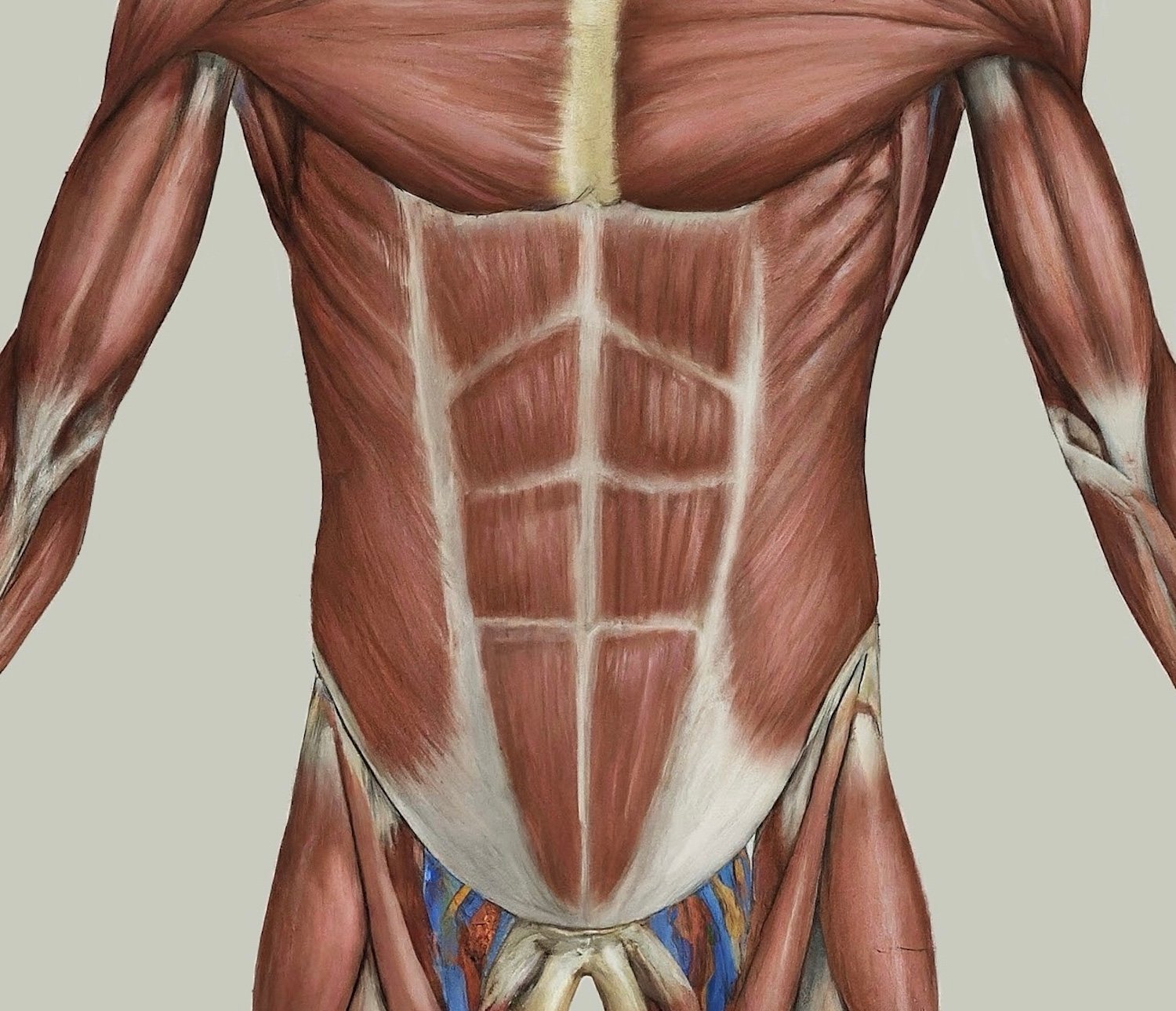
- Lateral musculature all form aponeurosis that inserts into the linea alba
- External oblique
- Fibers run inferomedially
- Medial extension forms anterior layer of rectus sheath
- Internal oblique
- Fibers run opposite of external oblique
- Transversus abdominis
- Fibers run transversely
- Extend medial to linea semilunaris, contributing to posterior rectus sheath
- External oblique
- Arcuate line
- Located 3 – 6 cm below the umbilicus
- Delineates point below which the posterior rectus sheath is absent
- Above the arcuate line, the internal oblique aponeurosis contributes to the anterior and posterior rectus sheaths and the transversus abdominis aponeurosis passes posterior to the rectus muscle to form the posterior rectus sheath.
- Below the arcuate line, the internal oblique and transversus abdominis aponeuroses pass only anterior to the rectus sheath. The posterior rectus sheath is composed of transversalis fascia and peritoneum only.
- Innervation: mostly intercostals nerves 7 – 12
- Blood supply
- Lateral abdominal muscles: lower 3 or 4 intercostal arteries, deep circumflex iliac artery, and lumbar arteries
- Rectus abdominis: superior epigastric artery (terminal branch of internal mammary), inferior epigastric artery (branch of external iliac), and lower intercostal
- Types of hernias
- Inguinal: protrusion of intraabdominal contents (usually fat) through the inguinal canal
- Indirect
- Most common type of hernia
- Most common hernia in women
- Protrudes from the internal inguinal ring obliquely toward the external inguinal ring into the scrotum and is lateral to the inferior epigastric vessels (lateral to Hesselbach’s triangle)
- Direct
- Protrudes outward and forward and is medial to the internal inguinal ring and inferior epigastric vessels
- Littre’s: inguinal hernia with a Meckel’s diverticulum in the hernia sac
- Indirect
- Ventral (abdominal): protrusion of intraabdominal contents through congenital or acquired defect in the abdominal wall
- Incisional: protrusion through previous surgical incision
- Umbilical: protrusion through the umbilicus
- Femoral
- Women more likely to get than men
- Intraabdominal contents herniate into femoral canal through femoral ring, below the inguinal ligament
- Hiatal: protrusion of any abdominal structure into thoracic cavity through lax diaphragmatic esophageal hiatus
- Internal: protrusion of visceral contents through congenital or acquired defect in peritoneum or mesentery within the abdominal cavity
- Pantaloon: when both indirect and direct hernias are seen at the same time
- Richter: protrusion of only a portion of the bowel circumference through a defect
- Spigelian: protrusion in the anterior abdominal wall adjacent to the semilunar line through a slit-like defect; almost all occur at or below the arcuate line
- Amyand: when the appendix is trapped within an inguinal hernia
- Parastomal: protrusion to side of stoma
- Acquired diaphragmatic: protrusion of intra-abdominal contents through abnormal opening in diaphragm
- Obturator: protrusion through obturator canal (formed by union of pubic bone and ischium)
- Lumbar: protrusion in lumbar region of posterior abdominal wall
- Interparietal: protrusion between layers of the abdominal wall
- Sciatic: protrusion through greater sciatic foramen
- Perineal: protrusion through pelvic diaphragm
- Inguinal: protrusion of intraabdominal contents (usually fat) through the inguinal canal
Complications
- Large hernias can result in loss of abdominal domain (when abdominal contents no longer reside in the abdominal cavity)
- Respiratory dysfunction
- Bowel edema
- Stasis of splanchnic venous system
- Urinary retention
- Constipation
Scoring Systems/Classifications
- Ventral Hernia Working Group grading scale
- European Hernia Society system

Differential Diagnoses
- Diastasis recti
- Abscesses
- Muscle strain
- Seroma
- Wound hematoma