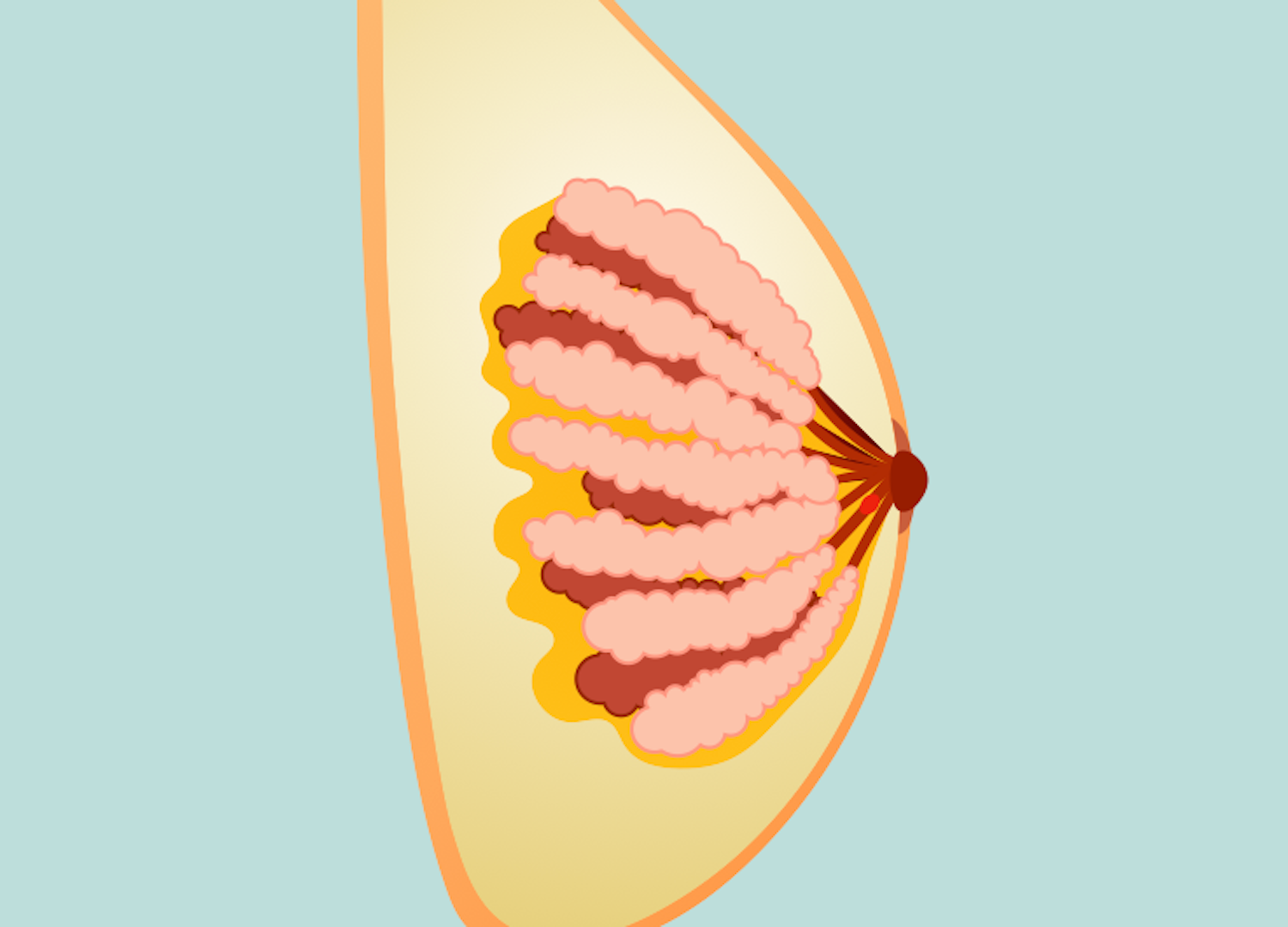
Intraductal papillomas are benign breast tumors that occur in breast milk ducts.
Etiology
- Risk factors
- Age 35 – 55
- Estrogen exposure
- Family history
Pathogenesis
- Epithelial cell overgrowth in breast milk ducts
History
- Asymptomatic
- Nipple discharge
- Breast lump
- Pain, discomfort
Physical Exam
- Usually < 1 cm (nonpalpable), but can grow 4 – 5 cm
- Often found behind the nipple
- Nipple discharge (clear or bloody)
Imaging
- Mammogram: round or oval mass with well-circumscribed or indistinct margin, may have microcalcifications
- Breast US: dilated duct
- Contrast ductogram
- Completed to located the papilloma
- Findings: intraluminal filling defect, ductal dilation leading up to the mass with abrupt ductal cutoff
- Biopsy
- Required for definitive diagnosis
- Core needle and vacuum-assisted biopsy are preferred
- Findings: fibrovascular core covered with epithelial and myoepithelial cells
Treatment
- Biopsy results will also influence treatment options. Presence or absence of atypia influences treatment decisions. If atypia is found, surgical excision is recommended. If atypia is not found, surgical excision may not be required.
- Solitary intraductal papillomas → observation or surgical excision
- Papillomatosis → surgical excision
- Surgical excision: subareolar resection of involved ducts and papilloma
Relevant Information
- Most common cause of bloody nipple discharge
- Benign: associated with development of DCIS (ductal carcinoma in situ)
- Intraductal papilloma subtypes
- Solitary papillomas
- Most common
- Single tumor that forms in the large milk duct near the nipple.
- No increased risk for breast cancer
- True polyps of epithelial-lined breast milk ducts
- Multiple papillomas (papillomatosis)
- Multiple papillomas in the smaller milk duct further away from the nipple.
- Increased risk for breast cancer risk
- Epithelial hyperplasia
- Not composed of true papillomas → composed of hyperplastic epithelium that may fill individual ducts similar to a true polyp, but has no stalk of fibrovascular tissue
- Solitary papillomas
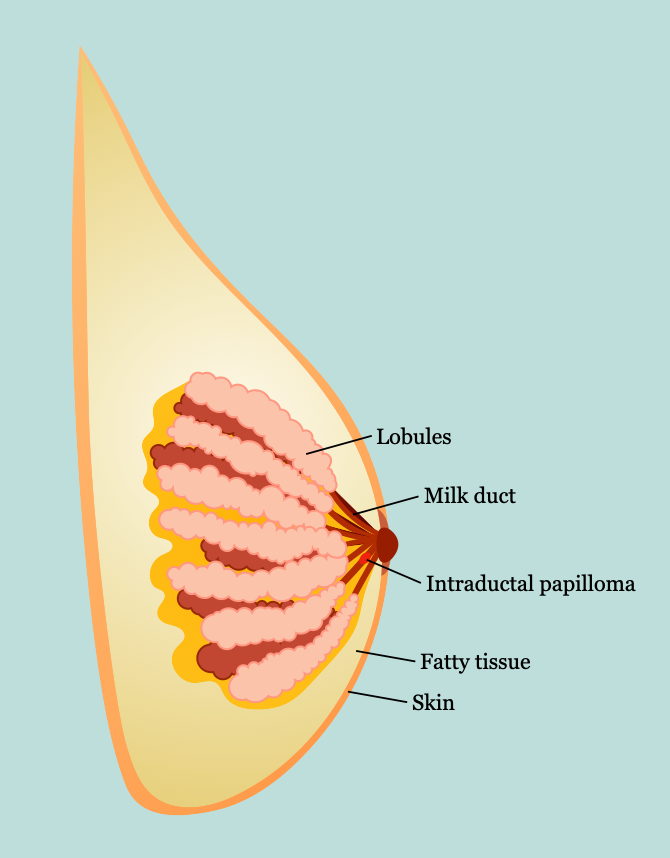
- Breast anatomy
- Lies between subdermal layer of adipose tissue and superficial pectoral fascia
- Cooper ligaments
- Provide structural support and shape (anchored into the skin)
- Infiltration by tumors can produce tethering, resulting in dimpling on the breast tissue
- Lymphatics
- Lymph nodes
- Level 1: located lateral to the lateral border of the pectoralis minor muscle
- Level II: located posterior to the pectoralis minor muscle as well as anterior to the pectoralis minor and posterior to the pectoralis major (Rotter or interpectoral nodes)
- Level III: located medial to pectoralis minor muscle and include subclavicular nodes
- Most drains to axillary nodes (97%)
- Any quadrant can drain into internal mammary nodes
- Supraclavicular nodes → N3 disease
- Primary axillary adenopathy → ≤ 1 is lymphoma
- Lymph nodes
- Nerves
- Long thoracic nerve
- Innervates serratus anterior muscle
- Injury → winged scapula
- Lateral thoracic artery supplies serratus anterior muscle
- Thoracodorsal nerve
- Innervates latissimus dorsi muscle
- Injury → weak arm pull-ups and adduction
- Thoracodorsal artery supplies latissimus dorsi
- Arises from posterior cord of brachial plexus; enters axillary space under axillary vein (close to long thoracic nerve)
- Medial pectoral nerve: innervates innervates pectoralis major and pectoralis minor muscles
- Lateral pectoral nerve: innervates pectoralis major muscle
- Intercostobrachial nerve
- Lateral cutaneous branch of second intercostal nerve
- Sensation to medial arm and axilla
- Most common injured nerve with modified radical mastectomy (MRM) or axillary lymph node dissection (ALND)
- Long thoracic nerve
- Arterial supply: branches of
- Internal thoracic (mammary) artery
- Intercostal arteries
- Thoracoacromial artery
- Lateral thoracic artery
- Batson’s plexus: valveless vein plexus, allows direct hematogenous metastasis of breast cancer to spine
- Costoclavicular ligament (Halsted ligament): defines axilla apex
- Breast development
- Formed from ectoderm milk streak
- Hormone influence
- Estrogen: duct development (double layer of columnar cells)
- Progesterone: lobular development
- Prolactin: synergizes estrogen and progesterone
- Cyclic changes
- Estrogen → increased breast swelling, growth of glandular tissue
- Progesterone → increased maturation of glandular tissue, withdrawal causes menses
- FSH, LH surge → ovum release
- After menopause, less estrogen and progesterone results in atrophy of breast and vulvar tissue
- Microscopic anatomy
- Three tissue types
- Glandular epithelium
- Branching system of ducts arranged in a radial pattern extending from the nipple-areolar complex
- Each major duct has branches and ultimately ends in terminal ductules or acini (acini are milk-forming glands of lactating breasts)
- Fibrous stroma and supporting tissues
- Adipose tissue
- Glandular epithelium
- Basement membrane
- Contains laminin, type IV collagen, proteoglycans
- Differentiates in situ from invasive breast cancer
- Three tissue types
Differential Diagnoses
- Breast cyst
- Galactocele
- Fibrocystic changes
- Breast abscess
- Phyllodes tumor
- Radial scar
- Intracystic carcinoma
Resources
- American Cancer Society. “Intraductal Papillomas of the Breast,” (2022)
- The American Society of Breast Surgeons. “Consensus Guideline on Concordance Assessment of Image-Guided Breast Biopsies and Management of Borderline or High-Risk Lesions,” (2018)