Appendicitis refers to inflammation of the appendix. The first appendectomy was completed by Claudius Amyand in 1735 when he operated on an 11-year-old male for a strangulated inguinal hernia and discovered the appendix in the hernial sac. The first intentional appendectomy was performed by Lawson Tait in 1880.
Etiology
- Luminal obstruction from various etiologies, leading to increased mucus production and bacterial overgrowth, resulting in wall tension and eventually necrosis and potential perforation
History
- Vague periumbilical abdominal pain, migrating to RLQ pain over time
- Anorexia
- Nausea
- ± Vomiting
- ± Diarrhea
- ± Constipation
Physical Exam
- Ill-appearing
- ± Fever
- Tachycardia
- Mild dehydration
- + McBurney’s sign
- Rebound tenderness
- Rigidity → if present, points towards perforation
- ± Rovsing sign
- ± Obturator sign
- ± Psoas sign
Labs
- WBC and inflammatory markers lack accuracy for diagnosis
- Leukocytosis, often with “left shift”
Imaging
- CT w IV contrast
- Most commonly used; effective and accurate; sensitivity 76-100%, specificity 83-100%
- Findings: thickened, inflamed appendix with surrounding “stranding” indicative of inflammation, > 7 mm in diameter, mural enhancement or “target sign”
- Xray → lack sensitivity and specificity
- US
- May have greater utility in pediatric or pregnant patients
- Success of study depends greatly on skill of the sonographer
- MRI w/o contrast
- Reserved for pregnant patients
- Criteria for MRI diagnosis: appendiceal enlargement (> 7 mm), thickening (> 2 mm), presence of inflammation
- Cons: higher cost, motion artifact
Treatment
- Appendectomy
- Fluid resuscitation, as indicated
- Broad-spectrum IV antibiotics
- Pain control: opioids, NSAIDs, acetaminophen
Relevant Information
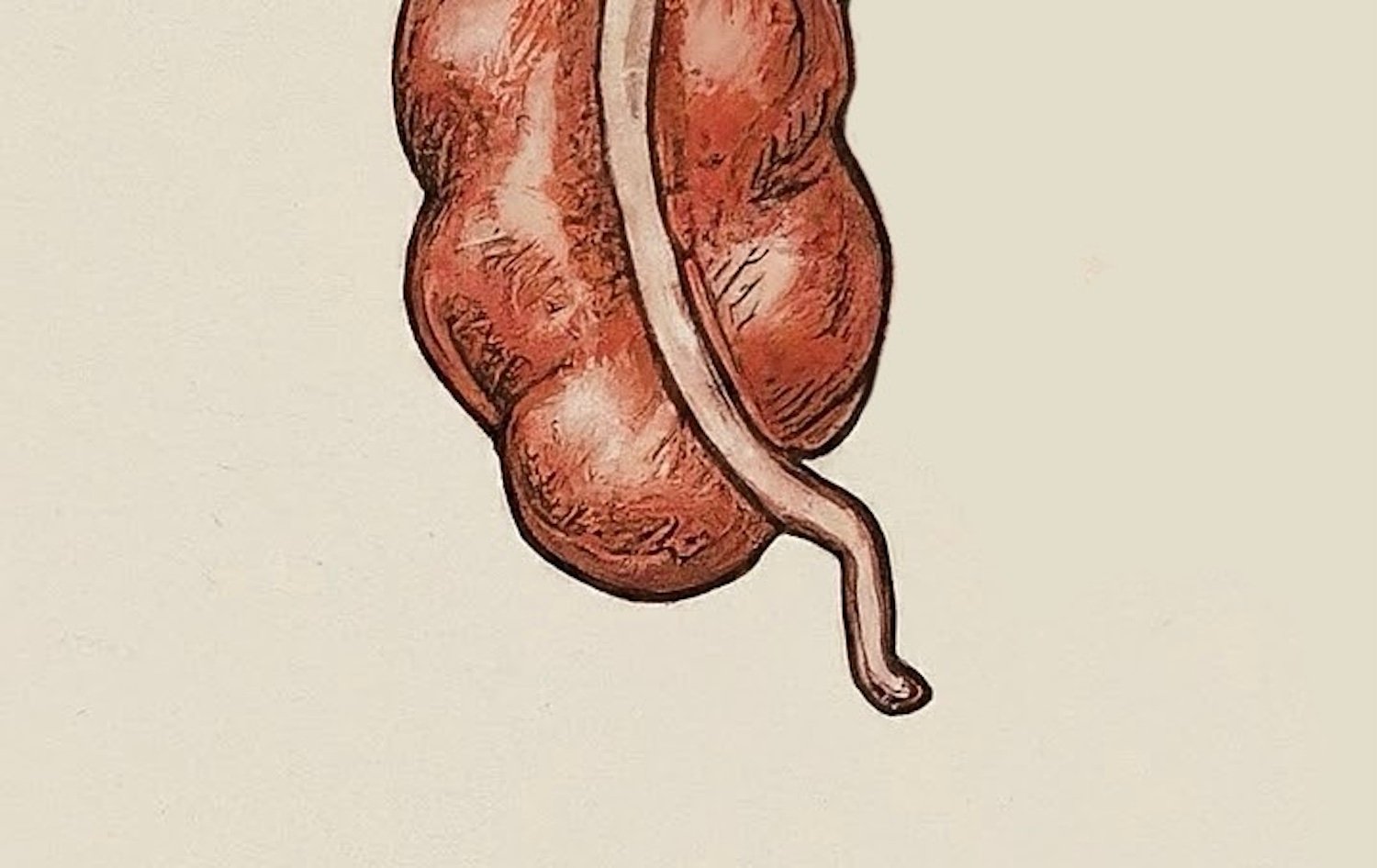
- Appendix orientation
- Retrocecal (65%)
- Pelvic (31%)
- Subcecal (2.3%)
- Preileal (1.0%)
- Retroileal (0.4%)
- Fold of Treves
- Bloodless fold; no sizable blood vessels
- Peritoneal structure that extends from the antimesenteric border of the terminal ileum to the base of the appendix, or anterior surface of the mesoappendix, or both
- Can aid in the recognition of the ileocecal region and base of the appendix
Complications
- Perforation: can lead to sepsis, increased risk with prolonged duration of symptoms; rigidity will be present upon physical exam
Scoring Systems
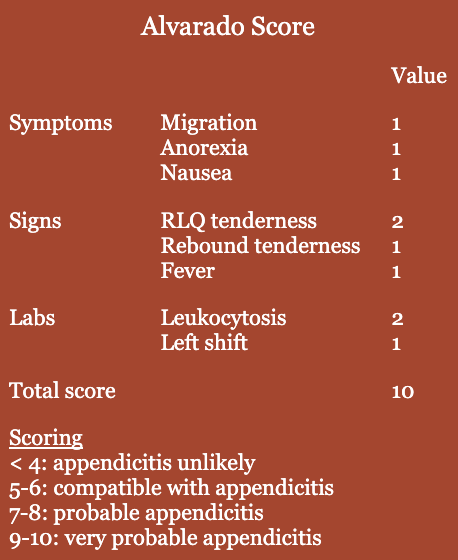
- No signs or symptoms have been shown to be uniquely predictive of appendicitis, so scoring systems have been developed to help with clinical diagnosis
- Alvarado scoring
- 8-item clinical and laboratory variables
- Scoring < 4 useful in excluding appendicitis; higher score lacks specificity
- Most widely used and acceptable
- Pediatric Appendicitis Score (PAS)
- Appendicitis Inflammatory Response Score (AIRS)
Differential Diagnoses
- Crohn ileitis
- Mesenteric adenitis
- Intussusception
- Meckel diverticulum
- Ectopic pregnancy
- Testicular torsion
- Ovarian torsion
- Kidney stones
- Gastroenteritis
- PID
- Endometriosis
- Renal colic
- Irritable bowel disease