Carotid endarterectomy (CEA) is a surgery performed in order to remove plaque buildup in the common carotid and internal carotid arteries in order to improve blood flow. It involves removing the diseased intima and media of the carotid artery. It was first performed successfully by Michael Ellis DeBakey in 1953. The first published report of carotid endarterectomy was in 1954 by Eastcott and others.

Indications
- Principal indications
- Transient ischemia → amaurosis fugax (due to occlusion of ophthalmic branch of ICA; temporary monocular blindness, “curtain coming down”), hemiparesis, facial weakness, speech loss
- Asymptomatic high-grade stenosis
- Symptomatic > 50% stenosis
- Asymptomatic > 70% stenosis
- Note
- Patients symptomatic < 50% stenosis → treat with Plavix, ASA, statin, optimize meds (NOT CEA)
- Patients asymptomatic 50 – 70% stenosis → treat with Plavix, ASA, statin, optimize meds
- Prevention of strokes in pts w systemic disease
- History of stroke in a patient who develops new symptoms
Contraindications
- Established long standing occlusion
- Neck radiation (relative)
Preoperative Considerations
- Carotid Duplex US blood-flow imaging studies ± MRA or contrast angiography
- Visualiz arch, carotids, and vertebral vessels
- Allows for accurate documentation of stenotic areas and the extent of disease in the collateral blood supply
- Delay procedure after stroke
- Delay 2 weeks if small, nonhemorrhagic stroke
- Delay 3 weeks if large, nonhemorrhagic stroke
- Delay 6 – 8 weeks if hemorrhagic stroke
- In patients with bilateral stenosis, repair is first completed on the most stenotic side
- If the patient has equally stenotic carotid stenosis bilaterally, repair is first completed on the dominant side
- Carotid artery stenting (CAS) may be preferred in patients with symptomatic carotid occlusion (55 – 99%) with multiple comorbidities, tracheostomy, prior neck radiation, or neck dissection, or in those unable to tolerate an open surgical procedure.
Risks
- Increased cerebral damage
- Hemiplegia
- Numerous postoperative complications (see below)
Relevant Anatomy
- Three large vessels arise from the aorta
- Brachiocephalic trunk → right common carotid artery, right subclavian artery
- Left common carotid artery
- Left subclavian artery
- Carotid sheath contents
- Carotid artery
- Internal jugular vein
- Vagus nerve (posterior 98%, anterior 2%)
- Deep cervical lymph nodes
- Common carotid artery
- Supplies 85% of blood flow to the brain
- Omohyoid muscle crosses the common carotid artery proximally
- Digastric muscle crosses the common carotid artery distally
- Carotid bifurcation
- Most common site of stenosis
- Carotid body
- Dissection → hypotension, bradycardia
- Avoid cardiovascular effects of dissection by injecting with 1% lidocaine
- Internal carotid artery (ICA)
- Continuous forward flow (biphasic, fast antegrade then slower diastolic antegrade)
- Continues into the skull to form part of the Circle of Willis
- Supplies blood to the brain and eyes
- First branch: ophthalmic artery
- External carotid artery (ECA)
- Triphasic flow (antegrade, retrograde, antegrade again)
- Supplies blood to the neck and face
- First branch: superior thyroidal artery
- Ophthalmic artery (off of ICA) and internal maxillary artery (off of ECA) allow for communication between ICA and ECA)

- Vagus nerve (CN X)
- Injury → vocal cord paralysis; hoarse (recurrent laryngeal nerve comes off of vagus)
- Most common nerve injury with CEA; from vascular clamping
- Hypoglossal nerve (CN XII)
- Injury → deviation of tongue to ipsilateral side and difficulty with mastication
- Crosses cephalad to the carotid bifurcation
- Ansa cervicalis (ansa hypoglossi)
- Branches from the hypoglossal nerve as it crosses internal carotid artery
- Passes inferiorly to innervate strap muscles
- Strap muscles
- Sternohyoid
- Sternothyroid
- Thyrohyoid
- Omohyoid

- Facial nerve (CN VII)
- Most cephalad extension of incision (should be well out of field anteriorly)
- Branches of facial nerve
- Temporal (frontal)
- Zygomatic
- Buccal
- Marginal mandibular
- Injury → droop corner of mouth (injury from retracting at angle of the jaw)
- Crosses internal carotid artery near the ear
- Cervical
- Glossopharyngeal nerve (CN IX)
- Injury → difficulty swallowing
- Facial vein
- Crosses the carotid bifurcation
- Branch off of internal jugular vein
- Can be divided safely
- Anterior triangle of neck
- Superior: inferior border of mandible
- Medial: midline of neck
- Lateral: anterior SCM
- Subdivisions: muscular, carotid, submandibular, and submental triangles
- Posterior triangle of neck
- Anterior: posterior SCM
- Posterior: anterior trapezius
- Inferior: middle ⅓ clavicle
- Subdivisions: occipital and supraclavicular triangles
- Vaso vasorum are the arteries that supply the blood vessel itself
Relevant Information
- Surgical improvement is minimal in patients with complete occlusion of the internal carotid artery
- One-stage bilateral carotid endarterectomy in patients with contralateral carotid occlusion isn’t recommended due to increased risk of complications. Carotid endarterectomies should take place 1 – 2 weeks apart.
- Tacking sutures
- Horizontal mattress sutures of 7-0 polypropylene placed at intervals circumferentially, using double-ended sutures placed from inside out and tied externally
- Often required to prevent subintimal disease
- Poiseuille’s law: the narrower the lumen of the vessel, the higher the flow rate through the stenotic segment
- Hollenhorst plaque: microemboli in retinal arterioles
Surgical Technique
- Patient is placed in the supine position with the head extended and turned toward the contralateral side. The neck and surrounding area is prepped and draped in the usual sterile fashion.
- Superiorly: mastoid process
- Anteriorly: angle of mandible
- Inferiorly: manubrium and clavicle
- Posteriorly: trapezius
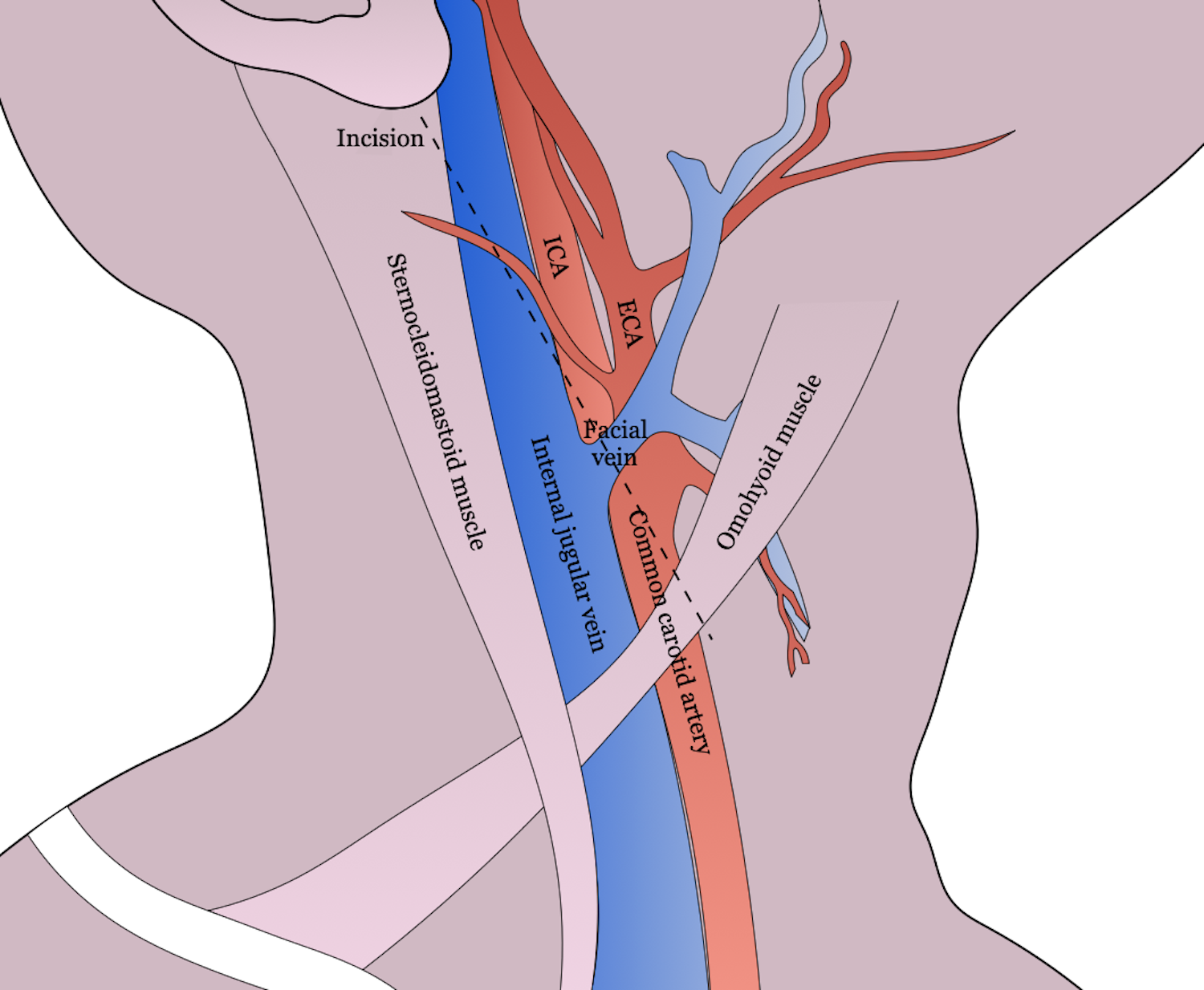
- The incision is made anterior to the sternocleidomastoid (SCM), from the mastoid process to a point ⅔ of the distance to the sternoclavicular joint. The incision is continued through the platysma, exposing the anterior border of the SCM. The anterior border of the SCM is retracted laterally to expose the carotid sheath.
- The marginal mandibular branch of the facial nerve is located anteriorly to the upper end of the incision, inferiorly to the horizontal ramus of the mandible, and must be avoided in order to prevent paralysis of the lower lip.
- The greater auricular nerve and sensory branches of the cervical plexus are located in the cephalad portion of the incision and must be avoided to preserve sensation to the earlobe and angle of the mandible.
- Self-retaining retractors may be placed to provide exposure. The omohyoid may be retracted inferiorly or divided to allow for exposure of the common carotid artery.
- The vagus nerve lies posterolaterally within the carotid sheath. The hypoglossal nerve passes superficial to the carotid arteries 1 – 2 cm cephalad to the carotid bifurcation. The ansa cervicalis (ansa hypoglossi) branches from the hypoglossal nerve as it crosses the internal carotid artery. The ansa hypoglossa may be divided to facilitate exposure to the more distal internal carotid artery, allowing the hypoglossal nerve to be redacted superiorly. The carotid body is at the crotch of the carotid bifurcation. The facial nerve is at the most cephalad of the incision and should be out of the field anteriorly.
- After exposure has been obtained, the facial vein is divided to expose the carotid bifurcation. The carotid sheath is entered and opened superiorly and inferiorly.
- A vessel loop is passed around the common carotid artery proximally.
- A vessel loop is passed around the external carotid artery to facilitate later placement of a vascular clamp.
- A vessel loop or 2-0 silk ligature is passed doubly around the superior thyroid artery as a Potts tie to provide vascular control.
- The internal carotid artery is dissected circumferentially 1 cm distal to palpable disease and encircled with a vessel loop. Great care is taken to prevent plaque embolization.
- Shunt. If a shunt is being used, equipment must be readied and flushed with saline to clear it of air and particular debris. Clamps are placed across the external carotid artery and common carotid artery, after which the needle is placed within the carotid artery to measure the carotid stump pressure. Pressures > 40 – 50 mmHg document significant collateral blood flow and are associated with a lower incidence of cerebrovascular accident. Extensive or ulcerated plaques need to be avoided to prevent plaque embolization. See articles below for more information on shunting.
- IV heparin is given by the anesthesiologist at the surgeon’s direction. Bulldog clamps are placed across the (1) internal carotid artery, (2) external carotid artery, and (3) common carotid artery in sequence. An incision is made on the anterolateral surface of the common carotid artery inferior to the bifurcation. The incision is elongated proximally and distally across the area selected for endarterectomy using Potts scissors. The arteriotomy must be extended distally to a point beyond the atheromatous plaque so that the endarterectomy can be performed entirely under direct vision. The incision is made through the thickened intima into the lumen. The line of cleavage is within the media, leaving the adventitia and media externa for closure.
- Shunt. If intraluminal shunting with a Pruitt-Inahara shunt is done, it needs to be flushed and prepared. Heparinized saline is flushed through the irrigating port and hemostats are placed on the proximal and distal limbs of the haunt directly adjacent to the irrigating port. The distal end is inserted first and the balloon is gently inflated to prevent bleeding around the shunt. The distal hemostat is then opened and the distal limb aspirated back through the irrigating limb to remove the air. The hemostat is reapplied. The proximal end of the haunt is inserted into the common carotid artery and the balloon is gently inflated to prevent antegrade flow through the shunt. Overinflation of the balloon can lead to tearing of the intaime, prolapsing of the balloon over the end of the shunt, and occluding flow. The proximal hemostat is removed and the limb is aspirated through the irrigating port to remove air and debris. The aspirating process should be repeated once more and the hemostats removed to establish flow through the shunt. The shunt is checked with Doppler to assess flow and the endarterectomy is then commended.
- Endarterectomy is begun, starting at the distal common carotid artery. A Freer elevator, blunt spatula, or mosquito hemostat is used. The correct endarterectomy plane is usually identified in the mid to outer media, leaving a smooth, shiny reddish-brown arterial wall behind. The dissection is continued carefully to elevate the plaque circumferentially. The plaque is then divided proximally with Potts scissors to facilitate exposure. The endarterectomy proceeds distally in a meticulous fashion with care taken to ensure a single endarterectomy plane. The most important part of the procedure is the delicate feathering of the endarterectomy at the distal boundary of the atheromatous plaque. A technical fault in the feathing will result in dissection after restoration of prograde flow with subsequent thrombosis and probably neurologic catastrophe. The plaque is removed in a similar fashion from the external carotid orifice by eversion endarterectomy allowing removal of the specimen. All residual debris is removed with forceps in a circumferential fashion. The field is irrigated with heparinized saline to allow for free removal of clot. Forceful irrigation distally may reveal elevation of distal flap which may require attention or tacking sutures.
- Occasionally, a very large artery with a short length arteriotomy can be closed primarily, however, patch angioplasty with prosthetic material (dacron, PTFE, or bovine pericardium) or autologous vein is the preferred technique for closure. Mattress sutures of double-ended 6-0 polypropylene are placed at either end. Both needles of each end suture pass through the patch from outside to in and then pass from lumen to the outside of the carotid artery where knots are tied. The inferior or proximal suture is run superiorly in a continuous manner on the medial side of the graft and tied to the other suture. Sutures on the lateral side are then run toward midpoint on the lateral side of the arteriotomy. When approximately 1 cm of arteriotomy remains to be closed in the midportion of the incision, the shunt is removed.
- Shunt. The balloons are deflated and a straight mosquito hemostat is used to cross clamp the shunt. A brisk inflow and backflow are allowed in order to flush the area as the two ends of the shunt are removed, first distally, then proximally. The bulldog clamps are reapplied or the vessel loops are cinched down to secure active bleeding.
- The remainder of the arteriotomy is closed rapidly, with care to flush the region of particulate debris and air. Once closure is complete, the clamps are removed in a specific order (1) external carotid artery, (2) common carotid artery, and (3) internal carotid artery in order to minimize the possibility of cerebral embolization, permitting potential emboli to be flushed into the external carotid system.
- Upon completion, a Doppler is performed to verify unobstructed blood flow. Many surgeons keep patients in the OR until they wake without any neurologic deficit. Re-exploration is completed if neurologic changes are present.
- Protamine sulfate is given to reverse anticoagulation (if heparin has been given). The wound is closed in layers, approximating the SCM and cervical fascia, platysma, and skin.
Intraoperative Complications
- Recurrent thrombosis
Postoperative Considerations
- Hypertension is avoided due to danger of acute stroke and disruption of the arterial closure
- Patient must be assessed for swallowing prior to self-feeding and discharge
- Patient started
- Dual antiplatelet therapy (e.g., aspirin, clopidogrel [Plavix])
- Statin
- Hypertension control
- Smoking cessation
Follow-up
- Carotid Duplex US
- Baseline should occur soon after the procedure (within 3 months) to establish post-operative baseline
- Every 6 months for 2 years and annually thereafter until stable (i.e., no restenosis or in-stent restenosis (ISR) observed in two consecutive annual scans)
- Some interval of regular surveillance (e.g., every 2 years) should be continued for the life of the patient due to the small risk of delayed restenosis or ISR
Postoperative Complications
- Nerve injuries: hypoglossal, vagus (most common nerve damage), glossopharyngeal, facial
- Myocardial infarction: most common cause of non-stroke morbidity and mortality following CEA
- Hyperperfusion syndrome
- Perioperative stroke
- Restenosis
- Death
- Transient ischemic attack
- Bleeding
- Infection
- Dysphagia
- Hematoma
Resources
- Society for Vascular Surgery. “Clinical Practice Guidelines for Management of Extracranial Cerebrovascular Disease,” (2021)
- Society for Vascular Surgery. “Guidelines on Follow-up After Vascular Surgery Arterial Procedures,” (2018)
- Cochrane Review. “Routine or Selective Carotid Artery Shunting for Carotid Endarterectomy,” (2022)
- Journal of Vascular Surgery. “Shunt Intention During Carotid Endarterectomy in the Early Asymptomatic Period and Perioperative Stroke Risk,” (2020)
- American Heart Association. “Impact of Shunting Practice Patterns During Carotid Endarterectomy for Symptomatic Carotid Stenosis,” (2022)
- North American Symptomatic Carotid Endarterectomy Trials (NASCET) (1999)