Breast cysts are fluid-filled, epithelial-lined cavities located within the breast parenchyma. They can range in size from microscopic to large palpable cysts with 20 – 30 mL of fluid.
Epidemiology
- Women
- > 35 years old
- Premenopausal
- Increases until menopause, then sharply declines
- New breast cyst formation in older women is associated with exogenous hormone replacement therapy
Pathogenesis
- 50% are multiple or recurrent
- Thought to arise from destruction and dilatation of lobules and terminal ductules
- Influenced by ovarian hormones
History
- Asymptomatic
- Breast mass that changes with menstrual cycle
- Variable size, larger size prior to menstruation and smaller in size after menstruation
Physical Exam
- Breast mass characteristics
- Soft
- Mobile
- Round
- Smooth
- Well circumscribed
Imaging
- Cyst can be confirmed by direct aspiration OR US
- Breast US
- Simple cyst
- Cyst with smooth borders, no solid intracystic components
- Always noncancerous
- Direct aspiration is not necessary
- Complex cyst
- Cyst with mix of fluid and solid intracystic components
- Direct aspiration may be necessary
- Complicated breast cyst
- Cyst with fluid; may have cloudiness to fluid or border may be irregular
- Direction aspiration may be used
- Simple cyst
- Direct aspiration
- Fluid can be straw-colored, opaque, or dark green and may contain debris
- If cyst resolves with aspiration and contents aren’t grossly bloody → fluid doesn’t need to be sent for cytologic analysis
- If cyst recurs multiple times (> 2 times) → core needle biopsy should be performed
- Core needle biopsy
- Evaluate solid elements
Treatment
- Usually doesn’t require treatment. Simple breast cysts usually resolve. Complex breast cysts may require aspiration and more follow-ups.
- Direct aspiration (see above)
- Surgical removal
- Isn’t usually indicated
- May be considered if cyst recurs multiple times or if needle biopsy reveals atypia, incompletely removes the mass, or if the cyst is large and painful
Relevant Information
- No evidence of increased risk for breast cancer
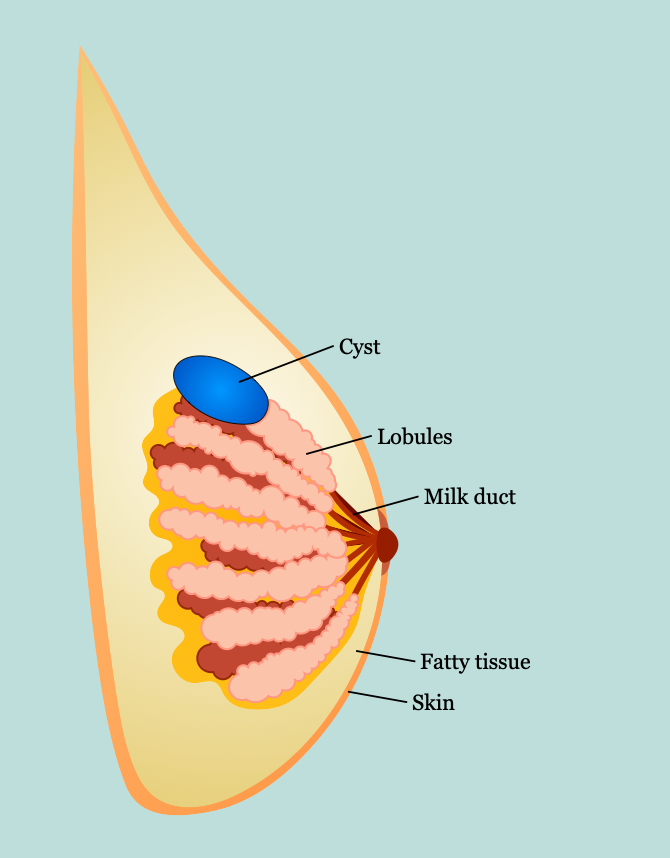
- Breast anatomy
- Lies between subdermal layer of adipose tissue and superficial pectoral fascia
- Cooper ligaments
- Provide structural support and shape (anchored into the skin)
- Infiltration by tumors can produce tethering, resulting in dimpling on the breast tissue
- Lymphatics
- Lymph nodes
- Level 1: located lateral to the lateral border of the pectoralis minor muscle
- Level II: located posterior to the pectoralis minor muscle as well as anterior to the pectoralis minor and posterior to the pectoralis major (Rotter or interpectoral nodes)
- Level III: located medial to pectoralis minor muscle and include subclavicular nodes
- Most drains to axillary nodes (97%)
- Any quadrant can drain into internal mammary nodes
- Supraclavicular nodes → N3 disease
- Primary axillary adenopathy → ≤ 1 is lymphoma
- Lymph nodes
- Nerves
- Long thoracic nerve
- Innervates serratus anterior muscle
- Injury → winged scapula
- Lateral thoracic artery supplies serratus anterior muscle
- Thoracodorsal nerve
- Innervates latissimus dorsi muscle
- Injury → weak arm pull-ups and adduction
- Thoracodorsal artery supplies latissimus dorsi
- Arises from posterior cord of brachial plexus; enters axillary space under axillary vein (close to long thoracic nerve)
- Medial pectoral nerve: innervates innervates pectoralis major and pectoralis minor muscles
- Lateral pectoral nerve: innervates pectoralis major muscle
- Intercostobrachial nerve
- Lateral cutaneous branch of second intercostal nerve
- Sensation to medial arm and axilla
- Most common injured nerve with modified radical mastectomy (MRM) or axillary lymph node dissection (ALND)
- Long thoracic nerve
- Arterial supply: branches of
- Internal thoracic (mammary) artery
- Intercostal arteries
- Thoracoacromial artery
- Lateral thoracic artery
- Batson’s plexus: valveless vein plexus, allows direct hematogenous metastasis of breast cancer to spine
- Costoclavicular ligament (Halsted ligament): defines axilla apex
- Breast development
- Formed from ectoderm milk streak
- Hormone influence
- Estrogen: duct development (double layer of columnar cells)
- Progesterone: lobular development
- Prolactin: synergizes estrogen and progesterone
- Cyclic changes
- Estrogen → increased breast swelling, growth of glandular tissue
- Progesterone → increased maturation of glandular tissue, withdrawal causes menses
- FSH, LH surge → ovum release
- After menopause, less estrogen and progesterone results in atrophy of breast and vulvar tissue
- Microscopic anatomy
- Three tissue types
- Glandular epithelium
- Branching system of ducts arranged in a radial pattern extending from the nipple-areolar complex
- Each major duct has branches and ultimately ends in terminal ductules or acini (acini are milk-forming glands of lactating breasts)
- Fibrous stroma and supporting tissues
- Adipose tissue
- Glandular epithelium
- Basement membrane
- Contains laminin, type IV collagen, proteoglycans
- Differentiates in situ from invasive breast cancer
- Three tissue types
Complications
- Infection
- Pain
Differential Diagnoses
- Fibrocystic changes
- Papilloma
- Breast abscess
- Phyllodes tumor
- Radial scar
- Intracystic carcinoma
