Supracondylar amputation is a type of above-knee amputation performed at the level of the thigh at the distal femur. The word amputation comes from the Latin amputātus, past participle of amputāre meaning to prune back or remove by cutting.
Wilhelm Fabry von Hilden (1560 – 1624) has been credited with performing the first amputation through the thigh
"Amputation or dismembering is the most lamentable part of surgery...if you be constrained to use your saw, let first your patient be well informed of the imminent danger of death by the use thereof."
-John Woodall (1556 - 1643)
Indications
- Trauma
- Poor blood supply
- Failure of reconstructive or bypass arterial procedures
- Unreconstructable circumstances as demonstrated with proximal and distal arteriography
- Tumor
- Progressive untreatable tumor
- Infection
- Emergency amputations: systemic complications or extensive infection
Preoperative Considerations
- Evaluate blood supply (e.g., arteriography), as it may eliminate need for amputation
- Determine if localized arterial obstruction
- Proximal obstruction → reconstructive procedure (e.g., iliac stent, aortofemoral) or distal bypass arterial graft (e.g., femoropopliteal)
- Infection
- Surgical debridement
- Antibiotics
- Delay amputation (if possible) if there is localized skin infection at the planned level of amputation
- Elective amputations may benefit emotionally and physically from preoperative consults with PT and a prosthetist
Relevant Anatomy
- Greater saphenous vein and nerve are in the subcutaneous tissue of the medial thigh. Lesser saphenous vein is in the subcutaneous tissue of the posterior leg and runs parallel to the sural nerve.
- Femoral artery
- Common femoral artery: proximal to origin of deep femoral artery
- Superficial femoral artery: distal to origin of deep femoral artery
- Profunda femoral artery (deep femoral artery)
- Usually arises from posterolateral aspect of femoral vein
- Tends to be the main channel after occlusion of the superior femoral vessels or a femoral-popliteal bypass graft
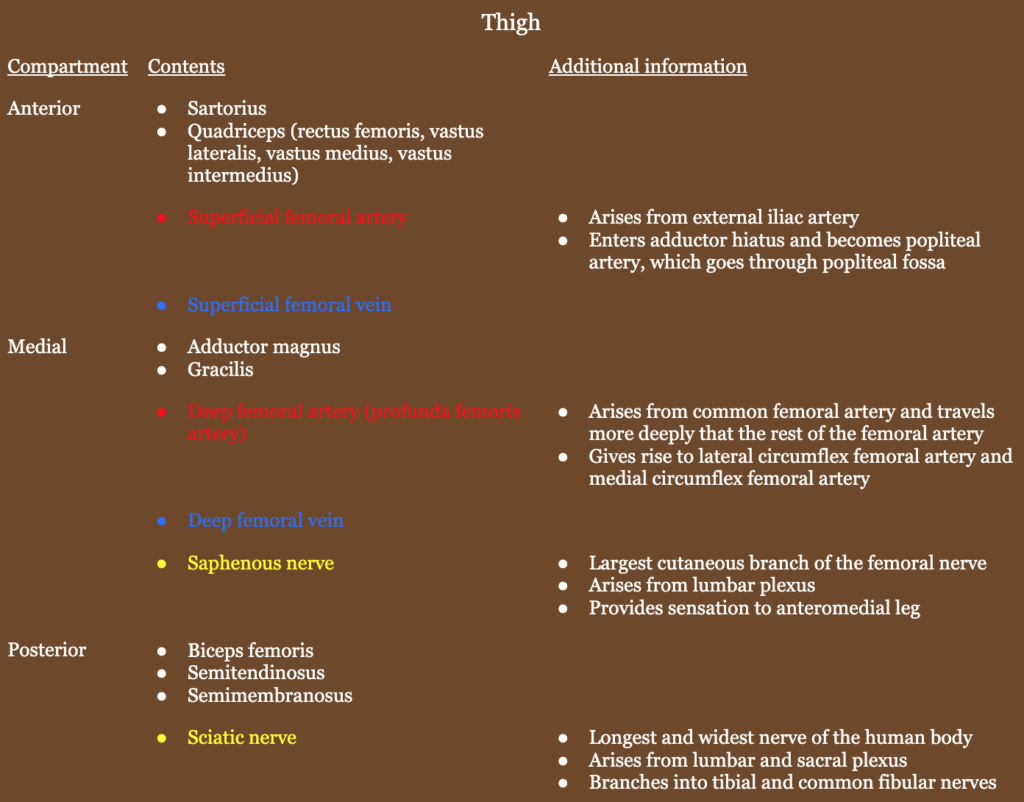
- Pes anserine (“goose’s foot” in Latin): conjoint tendon of sartorius, gracilis, and semitendinosus where they insert on anteromedial proximal tibia
- Popliteal artery
- Continuation of femoral artery
- Exits popliteal fossa under soleus muscle
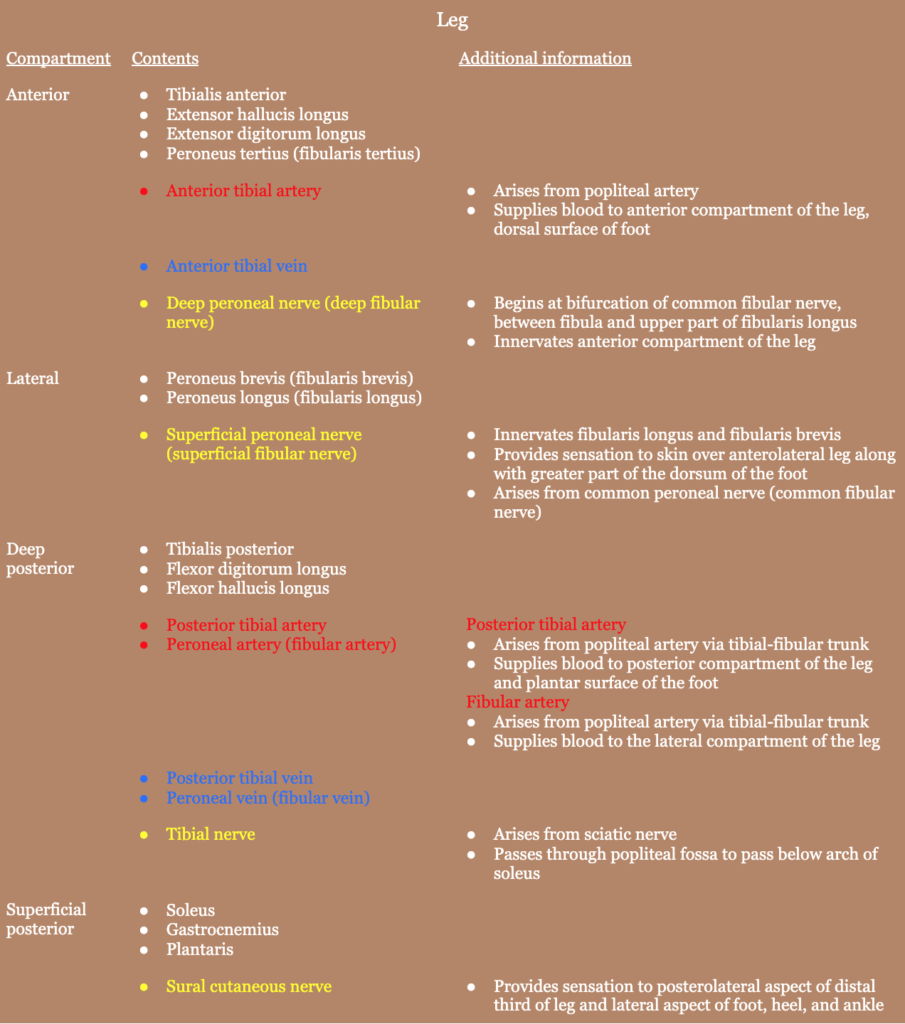
- Lower extremity nerves
- Obturator nerve: hip adduction
- Superior gluteal nerve: hip abduction
- Inferior gluteal nerve: hip extension
- Femoral nerve: knee extension
Relevant Information
- Sciatic nerve ligation: absorbable ligatures are avoided since they may be absorbed before the epineural sheath has united, causing the sheath to reopen and form a neuroma
- The best indicator of whether a patient will be able to walk with a prosthesis is if they were ambulatory prior to the amputation. Patients walking with crutches will probably be able to walk using a prosthesis.
Surgical Technique
- Patient is placed with the hip of the affected side out to the margin of the table, allowing for complete abduction of the thigh, with elevation of the calf or ankle with several sterile towels. The skin is prepped and a sterile sheet is placed beneath the thigh. A stockinette is placed on the foot and lower leg. Unless there is a progressive infection present, the extremity is elevated to encourage venous drainage. If a low amputation is planned, a sterile tourniquet can be applied high on the thigh.
- Type of flap that is used varies
- Progressive infection → circular incision is made for guillotine amputation
- No infection → anterior and posterior flaps
- Markings are made with a pen in order to ensure an appropriate stump length is made. Either equal anterior and posterior flaps are used, or a large anterior flap (most commonly) is used to place the scar away from the pressure points of the eventual prosthesis.
- The surgeon stands on the inner thigh to achieve better visualization of the main artery and nerves. Skin incision should extend 10 – 15 cm below the point where the bone is divided. The incision is carried through the skin and subcutaneous tissue down to the fascia over the underlying muscles.
- The most superficial vessel to be ligated is the great saphenous vein (medial/posteromedial aspect of the thigh), depending on the level of amputation. Muscles are divided at a level slightly higher than the skin and fascia and allowed to retract upward so the final flap will close with skin and fascia. The median incision into the muscle layer is made carefully and femoral vessels are identified deep to vastus medialis muscle. If a tourniquet has not been applied, major vessels can be identified by palpation. If a tourniquet has been applied, dissection is carried out until the femoral vein is visualized and then is subsequently divided between half-length clamps. The artery and vein are tied separately.
- The sciatic nerve, posterior to femoral vessels, is isolated from surrounding tissues. In a high amputation with a bifurcated sciatic nerve, the tibial and peroneal nerves are ligated individually. The ligation is carried out by pulling the nerve down as far as possible, applying a strong straight Ochsner clamp, applying a second similar crushing clamp 5 mm distal to the first, and the nerve is divided immediately below the second clamp. The proximal clamp is removed and the crushed area is ligated with a heavy, nonabsorbable 0 ligature. The distal clamp is removed, leaving a crushed and flattened short segment of nerve that tends to prevent the ligature from slipping off. The nerve retracts upward into the muscle, thus hopefully preventing the formation of a neuroma.
- The profunda femoris artery and vein must be secured and ligated in the posterior groups of muscles. The femur is circumferentially freed from surrounding soft tissue and the level of bone amputation is identified with preservation of good anterior and posterior skin flaps. A circular incision is made through the periosteum of the femur at the level of the amputation, and the inferior periosteum is elevated to allow for clean bone to be cut. Retraction and protection of the muscle are maintained while the femur is divided with a power saw at the identified level. The amputated limb is removed from the field.
- Sharp margins of the bone are beveled with a rongeur or rasp. If a tourniquet was used, it is removed at this time, and any bleeders are clamped and tied. The muscle is washed with warm isotonic saline until hemostasis is confirmed and all bone fragments are washed away. A deep drain may be placed if desired.
- Anterior and posterior flaps are inspected for length and trimmed as needed to ensure a snug (but not tight) closure. Deep investing fascia anteriorly and posteriorly are approximated with interrupted sutures over the end of the femur. Scarpa’s fascia is approximated with interrupted absorbable sutures to take tension off of the skin closure. If a guillotine type of amputation was carried out, the wound is left open to be closed later, or the limb may be reamputated at a higher level to allow for primary closure.
- Skin flaps are tailored to an appropriate shape and skin closure is performed. Interrupted, nonabsorbable monofilament sutures are used for closure without tissue ischemia.
- Once closed, the stump is covered with nonadherent dressing and fluffs of sterile gauze and is encased in a snug dressing. Since the stump will likely swell, the dressing is changed in 24 hours. An incisional vacuum sponge dressing along incision lines can be placed over nonadherent gauze if tissue edema is a big concern.
Postoperative Considerations
- The foot of the bed, but not the stump, may be elevated to combat swelling.
- Guillotine amputation
- Planned higher amputation → regular dressing changes performed until surgery
- Left to heal → progressive skin traction devices are applied to facilitate skin migration
- After initial healing of the wound, cotton-elastic bandages are wrapped around the stump to aid in shrinkage to allow for a prosthesis to be contoured. These bandages are changed every 4 hours
Postoperative Complications
- Phantom limb syndrome
- Normal part of recovery
- Often resolves with prosthesis
- Muscle atrophy
- Wound complications
- Infection
- Wound dehiscence
- Seroma
- Hematoma
- Risk factors: sepsis, compartment syndrome, ESRD, tobacco use, BMI > 30, BKA
- Phantom limb pain
- Depression
- Anxiety
- Death
