Choledocholithiasis occurs when there is a gallstone in the common bile duct. In 1877, Jean-Martin Charcot described the symptoms associated with the passage of common bile duct stones. Choledochotomy, or incision of the common bile duct, was practiced by several surgeons in the 1880s, including J.K. Thornton, Robert Abbe, Heussner, and H.O. Marcy. In 1890, L.J. Courvoisier was the first surgeon to operate specifically for the removal of common duct stones in a patient with prior cholecystectomy.
Etiology
- When bile isn’t completely drained from the gallbladder, it can precipitate as sludge, and then form into gallstones
- Primary vs. Secondary gallstones
- Primary: arise de novo in the gallbladder
- Secondary: pass from gallbladder into bile duct
- Types of gallstones
- Cholesterol stones (most common)
- Precipitates from cholesterol-rich bile
- NOT related to cholesterol levels in blood
- Color: light yellow to dark green, chalk white
- Pigmented (bilirubin) stones
- Form from breakdown of RBCs
- Color: dark black or blue
- Mixed pigmented stones
- Combination of calcium substrates, cholesterol, and bile
- Color: brown
- Cholesterol stones (most common)
- Risk factors: pregnancy, obesity, genetics, certain medications, gallbladder stasis, female sex, metabolic syndrome, rapid weight loss, prolonged fasting, bariatric surgery, Crohn disease
Epidemiology
- Seen in 10% of patients who have biliary imaging; incidental finding if asymptomatic
History
- Generally silent
- Biliary colic
- Obstructive jaundice: dark urine, scleral icterus, light stools
Labs
- Abnormal LFTs
Imaging
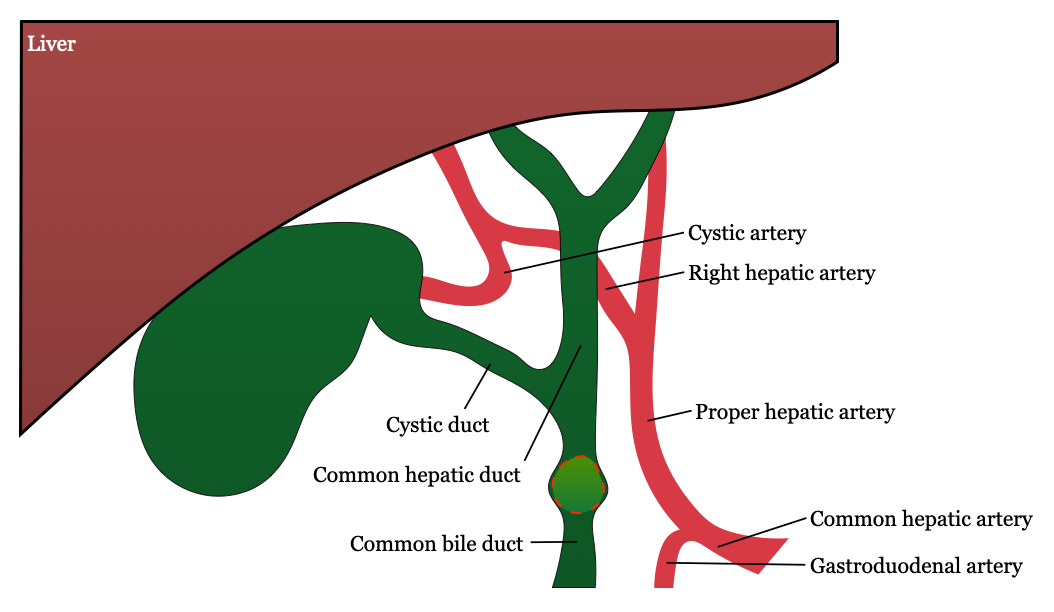
- RUQ US
- Best diagnostic test: 90% specificity
- Dilated bile duct (> 8 mm)
- MRCP
- Sensitive (> 90%) and specific (> 99%) in identifying CBD stones → most sensitive for detecting CBD stones
- Diagnostic only
- Done if there is a suspected stone in the CBD based on US results
- ERCP
- Also highly sensitive and specific for choledocholithiasis
- Often the therapeutic procedure due to clearing the duct. Gold-standard test if CBD stone is identified on MRCP
- Indications for preoperative ERCP
- Cholangitis
- Biliary pancreatitis
- Patients with multiple comorbidities
- Percutaneous transhepatic cholangiogram (PTC) can be used to treat choledocholithiasis in cases of unsuccessful ERCP
Treatment
- ERCP
- Over half of patients who undergo ERCP without cholecystectomy will have recurrence of biliary tract disease
- MCC of failure of ERCP: large gallstones (> 2.5 cm), altered gastric anatomy, and altered duodenal anatomy
- Cholecystectomy
Complications
- Cholangitis: ascending infection of CBD secondary to obstruction and increased intraluminal pressure
Notes
- LFT abnormalities on their own aren’t sensitive nor specific. A dilated bile duct in the presence of gallstones is suggestive of choledocholithisasis even if the patient doesn’t have symptoms
- Findings of choledocholithiasis during intraoperative cholangiogram can be managed either by CBD exploration or postoperative ERCP