Fistulas occur when there is an abnormal connection between two epithelialized surfaces that do not usually connect. Fistula-in-ano refers to a fistula between the skin and the anus. In 30 B.C., writings by Celsus advocated using a knife for treating fistula-in-ano. In cases where there were multiple openings, Celsus advocated for surgery in combination with ligature. John of Arderne (1307 – 1390 A.D.) described an operation for fistula-in-ano similar to treatments used today.
Etiology
- Anorectal abscess
- Cryptoglandular: anal crypts become blocked by inspissated debris/stool, infection develops at the anal glands which extends through the pathway of least resistance, abscess is formed in intersphincteric space leading to fistula development
- Postoperative or traumatic
- Inflammatory bowel disease
- Anal fissure
- Tuberculosis-related
- Risk factors: obesity, diabetes, smoking, hyperlipidemia, sedentary lifestyle
Pathogenesis
- Results from persistent communication between the anal canal (internal opening) and perianal skin (external opening) following spontaneous or surgical drainage
History
- Cyclical pattern of pain and swelling
- Drainage of the area associated with relief of symptoms
- Fecal soiling
- ± Bleeding
Physical Exam
- ≥ 1 external opening with or without granulation tissue
- Multiple external openings (“watering can perineum”) → suspicious for perianal Crohn disease
- External opening on the anal margin skin with heaped-up granulation tissue tender to palpation
- Digital rectal exam: palpation of a cord-like subcutaneous structure
- Location of the fistula can help diagnose the type of fistula. Goodsall’s rule can be used to help locate the internal opening as well.
- Submucosal: external opening in posterior midline close to anal verge
- Intersphincteric: external opening off the midline close to anal verge
- Low transsphincteric: external opening in anterior location
- Transsphincteric or suprasphincteric: external opening in ischiorectal fossa
- Draining of fistula tract
Imaging
- Anoscopy
- Direct inspection of dentate line
- May reveal an erythematous crypt or visible internal opening
- Can help exclude inflammatory conditions
- Exam under anesthesia
- Routine imaging is not usually necessary. It may be considered in patients with recurrent or complex anal fistula, immunosuppression, or anorectal Crohn disease.
- MRI pelvis
- Identify primary and secondary openings
- Delineate anatomy of fistula tracks
- Endoanal US (EAUS)
- Transperineal US (TPUS)
Treatment
- Goals for treatment
- Eliminate sepsis
- Remove or ablate epithelialized tracts
- Avoid or minimize the risk of fecal incontinence
- Prevent recurrence
- Lay-open technique (fistulotomy)
- Indications: simple fistula-in-ano with normal anal sphincter function
- Recurrence and incontinence are most significant complication
- Risk factors for postoperative anal sphincter dysfunction: preoperative fecal incontinence, recurrent fistula, female sex, complex fistulas, previous anorectal surgery, women with anterior fistulas or who have occult sphincter damage from previous birthing trauma
- Seton
- Indications
- Greater than lower ¼ of external anal sphincter involved (for first procedure) followed by either LIFT or anorectal advancement flap
- When lay open technique is not possible or not advisable
- Complex cryptoglandular anal fistulas
- Used to control the fistula: narrow the fistula tract and prevent recurrent cyclical symptoms, shorten fistula track
- Indications
- Endorectal advancement flap (ERAF)
- Indications
- High transsphincteric fistulas
- Suprasphincteric fistulas
- Involves curettage of fistula tract, sutured closure of internal opening, and covering of the internal opening with a mobilized segment of the rectum
- Indications
- Ligation of intersphincteric fistula (LIFT)
- Indications
- Simple fistulas
- Complex fistulas
- Transsphincteric fistulas
- Identification of internal opening with suture ligation of intersphincteric portion of the fistula. Tract and gland are excised and the wound is debrided.
- Indications
- Fibrin glue → relatively ineffective
- Anal fistula plug → relatively ineffective
Relevant Information
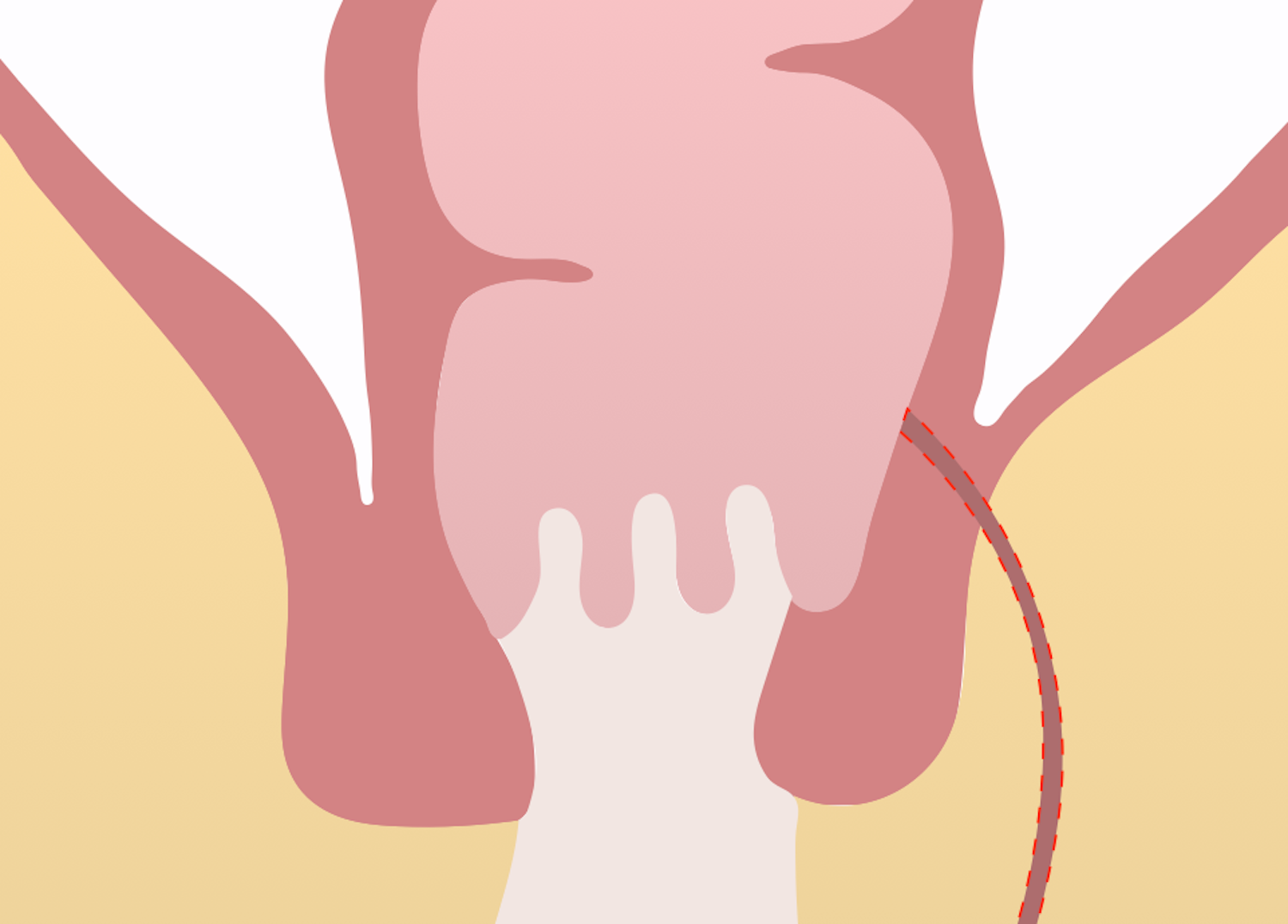
- Goodsall’s rule: predict the course of the fistula tract and location of the internal opening; help locate internal opening
- Fistulas with an external opening anterior to the anus connect with anus/rectum in a straight line
- Fistulas with an external opening posterior to the anus go toward a midline internal opening in the anus/rectum in a curvilinear fashion
- Anal canal
- Connection between the anal verge and anorectal junction; 2 – 4 cm in length
- Dentate line lies midpoint in the anal canal
- Proximal: longitudinal folds of columnar epithelium (columns of Morgagni)
- Distal: smooth squamous epithelium (anoderm)
- Anal crypts are located between the columns of Morgagni, where anal ducts empty
Classifications
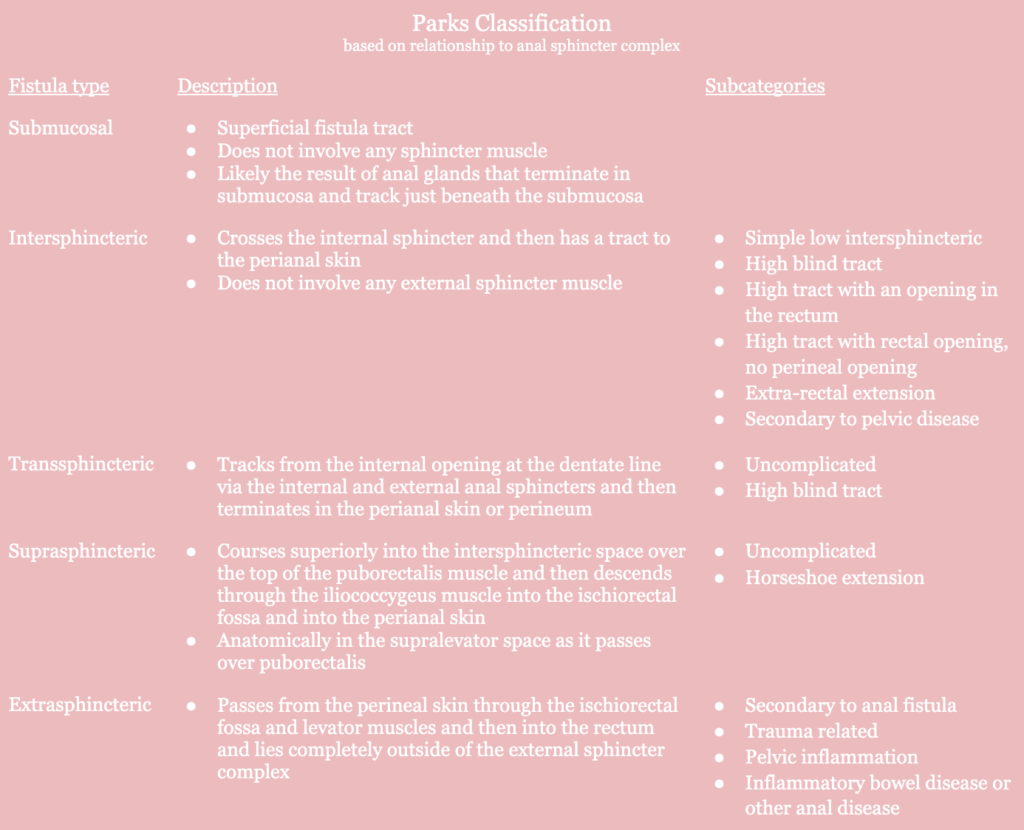
- Simple vs. complex
- Simple fistula
- Due to glandular obstruction resulting in anorectal abscess, and ultimately, a fistula
- Single tract, subcutaneous tract, involve < 30% of the external sphincter
- Complex fistula
- Any fistula that is high transsphincteric or when a fistulotomy would result in incontinence
- Includes suprasphincteric, extrasphincteric, all anterior transsphincteric fistulas in women, fistulas caused by Crohn disease, malignancy, surgery, and trauma
- Simple fistula
Differential Diagnoses
- Acute proctitis
- Anal carcinoma
- Anorectal abscess
- Constipation
- Diverticulitis
- Hidradenitis suppurativa
- Inflammatory bowel disease
- Pilonidal cyst
Resources
- American Society of Colon and Rectal Surgeons. “Clinical Practice Guidelines for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula,” (2022)