Pain management has often been considered the fifth vital sign. Making sure patient’s pain is under control is incredibly important in improving their outcomes. Frequent assessment of patient’s pain and their current pain regimen should be a daily occurrence. There are a lot of options when it comes to managing and treating patient’s pain, all of which should start with patient education and managing their expectations. As far as selecting what type of pain regimen to use, multimodal therapy, which uses a nonpharmacologic and multiple pharmacologic therapies (with the foundation being nonopioids), is most beneficial.
Pain Assessment
- Kids: Wong-Baker Faces
- Adults: pain scale of 0 (“no pain at all”) to 10 (“worst pain of your life”)
- Ventilated/nonverbal: facial expressions, guarding, agitation, irritability, vocalization, changes in ventilator compliance
- Physical exam: tachycardia, hypertension, tachypnea
Management
- Begins with a conversation with the patient to help manage expectations, with additional of the below interventions as needed
- Nonpharmacologic
- Cold packs
- Heat packs
- Cognitive strategies (questionable evidence)
- Pharmacologic
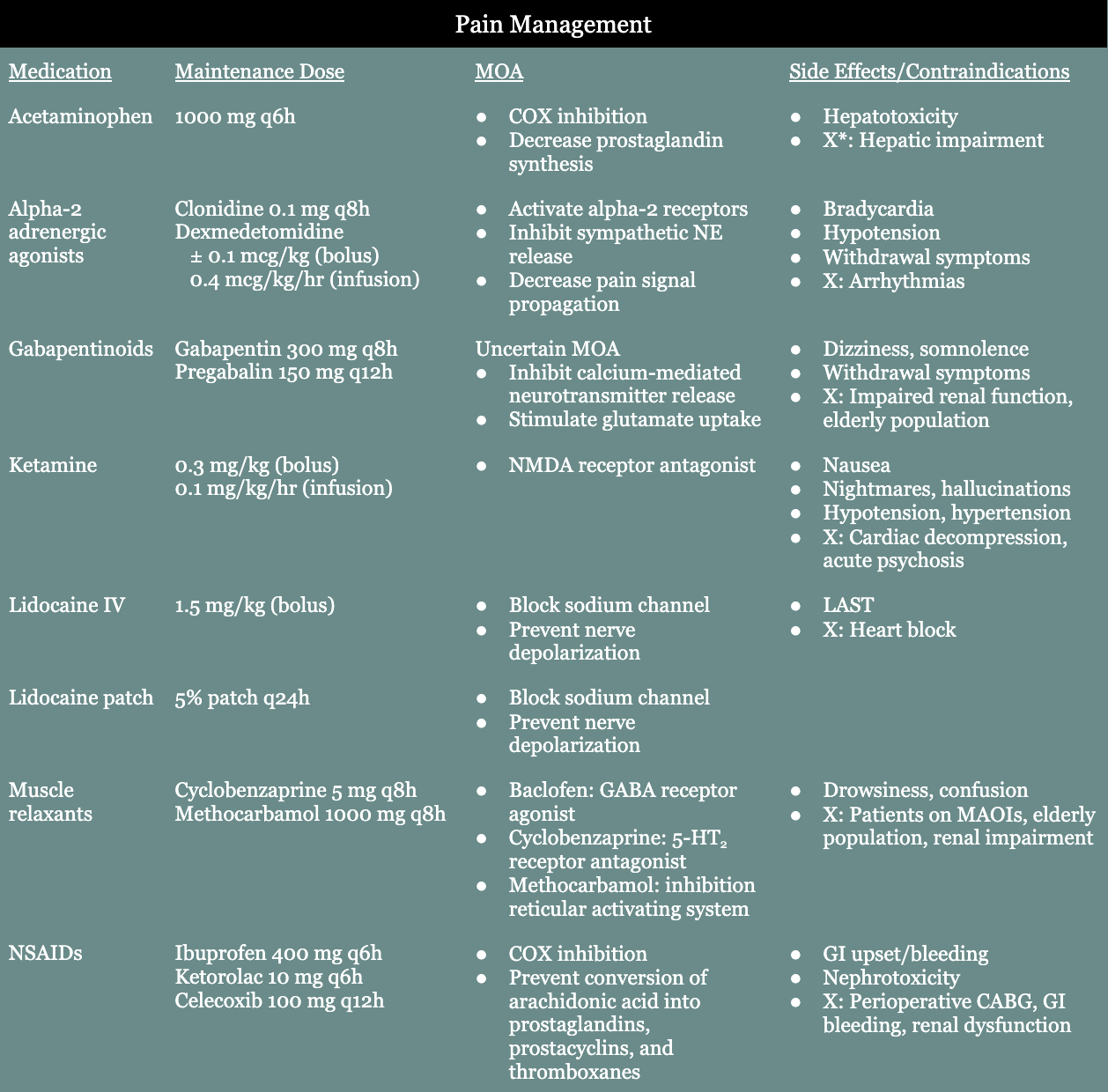
- Nonopioids
- Acetaminophen
- Alpha-2 adrenergic agonists (i.e., clonidine, dexmedetomidine)
- Gabapentinoids (i.e., gabapentin, pregabalin)
- Ketamine
- Lidocaine IV infusion
- Lidocaine patches
- Muscle relaxants (i.e., baclofen, cyclobenzaprine, methocarbamol)
- NSAIDs (i.e., ibuprofen, ketorolac, naproxen, celecoxib, aspirin)
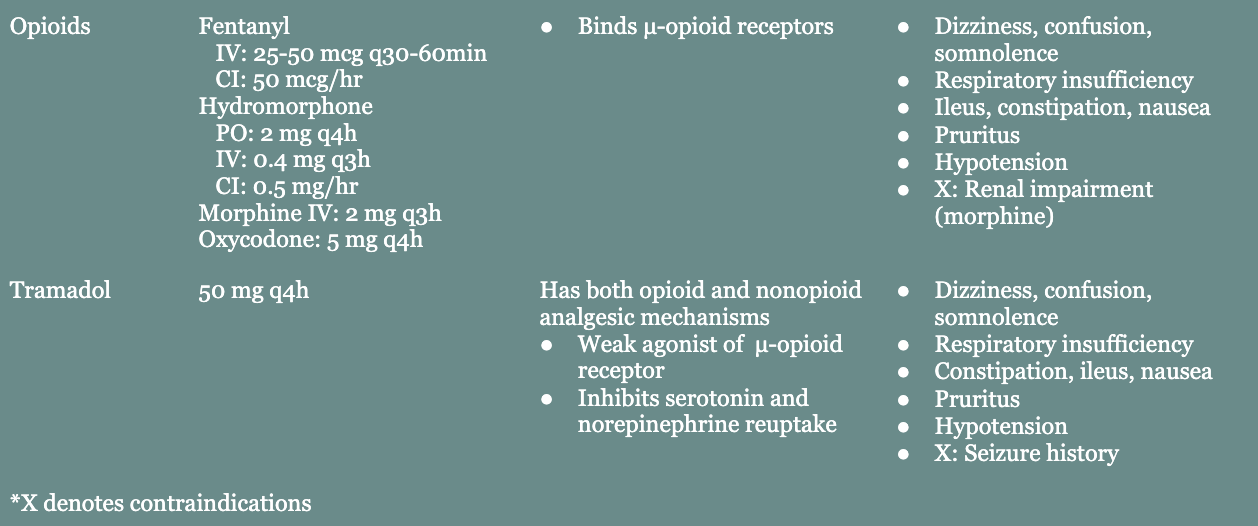
- Tramadol: has both opioid and nonopioid analgesic mechanisms
- Opioids
- Fentanyl
- Hydromorphone
- Morphine
- Oxycodone
- Regional anesthesia
- Neuraxial (i.e., epidural, spinal)
- Primary agents: local anesthetics, opioids
- Contraindicated in patients who are anticoagulated, have spinal cord injuries, or depressed mental status
- Peripheral (i.e., blocks, catheters, local wound infiltration)
- Primary agents: local anesthetics (i.e., lidocaine, bupivacaine)
- Blocks
- Abdominal: rectus sheath, ilioinguinal iliohypogastric, transversus abdominis plane
- Paraspinal: paravertebral, erector spinae
- Chest wall: serratus anterior, parasternal intercostal
- Extremity: brachial plexus, sciatic, femoral
- Neuraxial (i.e., epidural, spinal)
- Nonopioids
Resources
- American College of Surgeons (ACS) Best Practice Guidelines for Pain Management in Trauma Patients (2020).
- Enhanced Recovery After Surgery (ERAS) Society Guidelines for Perioperative Care.
