Rectovaginal fistulas are an abnormal connection between the rectum and vagina. In patients with recurring or persistent rectovaginal fistulas, a Martius repair can be utilized to correct the abnormality. This technique was first described in 1928 by Heinrich Martius, a German Ob/Gyn.
Etiology
- Obstetric complications (most common cause)
- Third- or fourth-degree laceration repair dehiscence (breakdown of repair appears 1 – 2 weeks after delivery)
- Unrecognized vaginal laceration during operative vaginal or precipitous delivery (instrumentation injury appears immediately)
- Inflammatory bowel disease
- Crohn disease (common)
- Ulcerative colitis is less common since it isn’t transmural
- Infection
- Cryptoglandular abscess (commonly located in anterior aspect of anal canal)
- Lymphogranuloma venereum
- Tuberculosis
- Bartholin gland duct abscess
- HIV
- Diverticular disease
- Previous surgery in anorectal area
- Hemorrhoidectomy
- Low anterior resection
- Excision of rectal tumors
- Hysterectomy
- Posterior vaginal wall repairs
- Pelvic radiation therapy
- Neoplasm
- Invasive cervical or vaginal cancer
- Anal or rectal cancer
- Trauma
- Intraoperative
- Coital
Pathogenesis
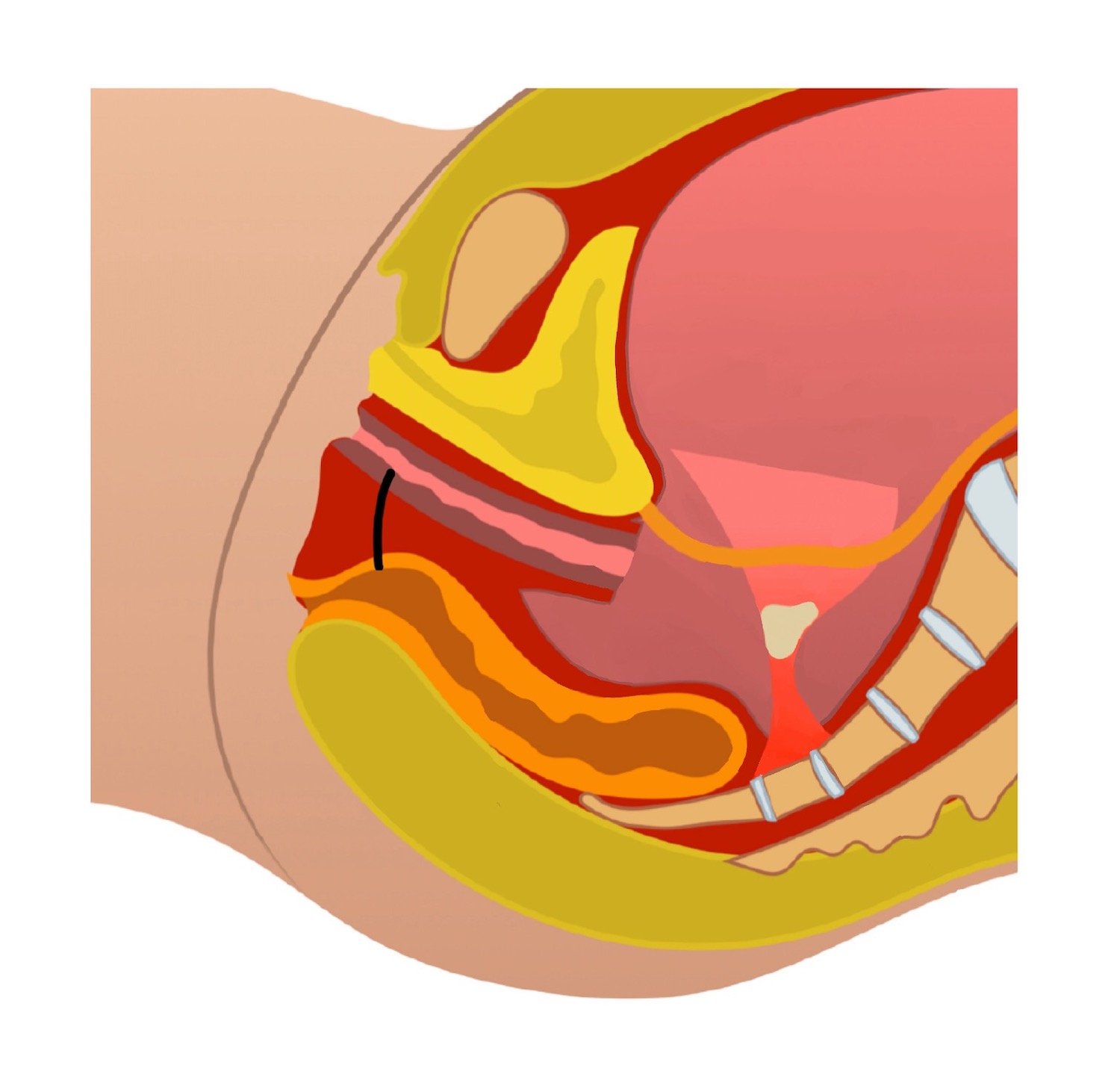
- Epithelial-lined communication between the rectum and vagina
History
- Occasional passage of flatus through the vagina
- Continuous drainage of stool through the vagina
- Recurrent bladder or vaginal infections
- Rectal or vaginal bleeding
- Obstetric etiologies may present with gross fecal incontinence
- Infectious or inflammatory etiologies may present with abdominal cramping and fevers
Physical exam
- Undrained abscess or purulent perineal drainage
- Location of fistula in relation to sphincter muscles and pelvic floor should be noted as this can affect the repair technique
- Palpable fistula tract
- Air bubbles at fistula’s vaginal opening after filling te vagina with water (done if initial examination doesn’t reveal readily seen fistula)
Imaging
- Consider imaging and other etiologies if rectovaginal fistula is not identified on exam
- Exam under anesthesia
- Barium enema
- CT with IV and rectal contrast
Treatment
- Repair of rectovaginal fistulas from obstetric injury tends to be more successful compared to other etiologies
- Surgical repair
- Depending on etiology, such as inflammatory, recommended 3 – 6 months after disease onset (to decrease inflammation in tissues and increase likelihood of a successful repair)
- Draining seton, antibiotics, or fecal diversion are considered depending on size, location, and etiology of the fistula
- Repair techniques
- Endorectal advancement flap
- Most popular surgical repair
- Fistula tract excision and closure of rectal portion of the fistula with a vascularized mucosal flap
- Transperineal repairs
- Episioproctotomy with layered closure
- Transperineal repair with levatorplasty
- LIFT procedure
- Sphincteroplasty
- Tissue transposition repairs
- Labial fat pad interposition (Martius flap)
- Gracilis muscle interposition
- Transvaginal repairs
- Transabdominal repairs
- Endorectal advancement flap
Complications
- Fecal incontinence
- Vaginal, perineal, or anal irritation
- Abscess
- Fistula recurrence
Differential Diagnoses
- Inflammatory bowel disease
- Colon cancer
- Large bowel disease
- Malignancy
- Surgical complications
Resources