Modified radical mastectomy is the surgical removal of the entire breast, including the nipple-areolar complex, majority of excess skin, and level I and II axillary lymph nodes. It may also be referred to as a total mastectomy with axillary lymph node dissection. It began to be widely accepted as a form of treatment and became more accepted as a standard of care in the 1970s.
Charles Hewitt Moore (1821-1870) wrote in 1867 that “recurrence of breast disease is due to inadequate removal within the breast and the entire breast, skin (if needed), and diseased axillary glands should be taken away.” Later on, William Halstead (1890) wrote about removing the breast while also cleaning out the axilla and taking out most, if not all, of the pectoralis major.
Indications
- Large breast cancer in relation to breast size, making cosmesis difficult
- Inflammatory breast cancer (following neoadjuvant chemotherapy)
- Multicentric cancers
- Patient preference
Preoperative Considerations
- Evaluate contralateral breast
- Genetic testing
- Use of short-acting muscle depolarizing agents should be used for intubation so that motor nerve responsiveness can be assessed during axillary node dissection
Relevant Anatomy
- Breast borders
- Superior: clavicle
- Inferior: inframammary fold
- Medial: sternum
- Lateral: latissimus dorsi
- Axillary borders
- Anterior: pectoralis minor, pectoralis major
- Superior: axillary vessels, clavicle, scapula, rib 1
- Medial: serratus anterior, ribs 1-4
- Lateral: humerus, coracobrachialis, short head of biceps brachii
- Posterior: latissimus dorsi, subscapularis, teres major
- Cooper’s ligaments
- Suspensory ligaments that divide breast into segments
- When breast cancer involves these strands, it can result in dimpling of the skin
- Breast blood supply
- Internal thoracic (mammary): 2nd, 3rd, 4th perforating arteries
- Lateral thoracic
- Thoracoacromial
- Posterior intercostal arteries: 2nd, 3rd, 4th
- Batson’s plexus → valveless veins that drain to vertebral blood supply
- Lymph node levels
- Level I: lateral to pectoralis minor
- Level II: beneath pectoralis minor
- Level III: medial to pectoralis minor
- Level I and II are targets for axillary dissection
- Breast innervation: lateral and anterior cutaneous branches of intercostal nerves 3, 4, 5
- Nerves
- Long thoracic nerve
- Innervates serratus anterior (lateral thoracic a. supplies serratus anterior)
- Injury → winged scapula
- Thoracodorsal nerve
- Innervates latissimus dorsi thoracodorsal a. supplies latissimus dorsi)
- Injury → weak arm pull-ups and adduction
- Medial pectoral nerve
- Innervates pectoralis major and pectoralis minor
- Passes through pectoralis minor in 60% of patients and passes laterally around pectoralis minor in 40% of patients as it travels to innervate the lower region of the pectoralis major
- Arises from medial cord of brachial plexus
- Lateral pectoral nerve
- Innervates pectoralis major
- Dominant lateral nerve to pectoralis major muscle arises from lateral cord and passes medial to pectoralis minor near its insertion; closely associated with acromial thoracic artery
- Intercostobrachial nerve (lateral cutaneous branch of 2nd intercostal nerve)
- Provides sensation to medial arm and axilla
- Located just below axillary vein during axillary dissection
- Can transect without serious complications
- Most common injured nerve in modified radical mastectomy or axillary lymph node dissection
- Long thoracic nerve
Surgical Technique
- Patient is placed in the supine position with the arm abducted at a right angle to allow for access to the axilla. The skin is prepped widely to include the involved breast, sternum, supraclavicular region, shoulder, axilla, collateral chest wall, and upper abdomen on the involved side. The hand is often wrapped in a sterile dressing. The patient is then draped in the usual fashion.
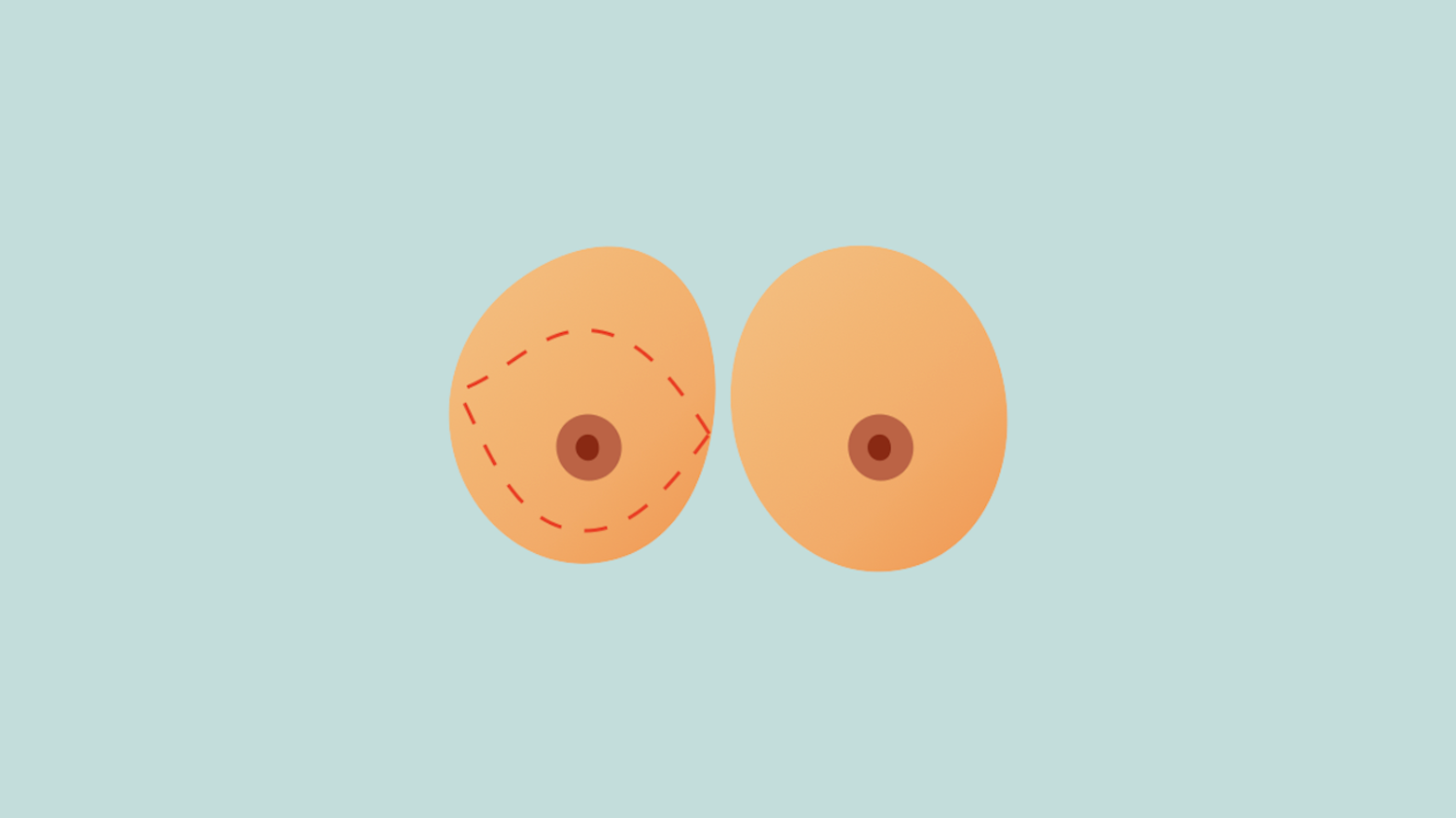
- An oblique elliptical incision is made with an extension laterally up toward the axilla for better visualization during axillary dissection with a better cosmetic closure. The transverse segment of the elliptical incision includes the nipple and areola with an appropriate distance beyond the limits of the tumor when possible. A more conservative incision that preserves skin is made when reconstruction is planned, and the incision can be planned with the plastic surgeon.
- The initial incision should be made only through the dermis in order to include as much subcutaneous tissue with the final specimen as possible. The skin flaps require careful elevation – with good retraction, a plane between the breast tissue and subdermal fat can be visualized. Dissection is carried out in this plane to ensure removal of all possible breast tissue while maintaining viability of the skin.
- The flaps are elevated to the level of the clavicle superiorly, to the edge of the sternum medially, to the rectus sheath and costal margin inferiorly (some surgeons prefer elevation to the level of the inframammary fold when reconstruction is planned), and to the latissimus dorsi laterally. Because lymph nodes and breast tissue are very close to the skin at the axilla, as much subcutaneous fat is removed from this area as is possible.
- Fascia over the pectoralis major as well as the breast is resected as a subfascial dissection starting near the clavicle and extending downward over the midportion of the sternum. Perforating intercostal arteries and veins near the sternal margins must be carefully clamped and ligated.
- The axillary flap is retracted upward and the fascia over the edge of the pectoralis major is incised, exposing the pectoralis minor below, and the junction of the coracobrachialis and pectoralis minor origins superiorly at the coracoid process. The loose tissue overlying the axillary vein is incised and the vein wall is gently exposed beyond the subscapular vessels.
- Level I and II lymph nodes are removed in the axillary node dissection which begins by incising the clavipectoral fascia along the lateral edge of the pectoralis minor. Caution is used to avoid the medial and lateral nerves to the pectoralis major. Lateral edge of pectoralis minor is cleared of fascia to near its insertion on the corticoid process and several veins are ligated as they drain into the axillary vein. Pectoralis major and minor are retracted upward and medially to expose the uppermost tissues to be divided over the axillary vein.
- Fascia overlying the serratus anterior is dissected free and the axillary fat and lymph nodes are mobilized off the chest wall and axillary vein. The long thoracic nerve should be identified deep to the axillary vein, as it lies within the loose fascia over the serratus anterior muscle and is possible to lift away from the muscle and divided. The more transverse intercostobrachial nerve appears beneath the second rib provides sensation to the upper inner aspect of the arm and is often sacrificed during axillary dissection.
- As the breast is retracted laterally, the long thoracic nerve and thoracodorsal nerve should be free of redundant tissue. The thoracodorsal nerve is located adjacent to the deep subscapular vein and artery. Division of this nerve is avoided unless the tumor is involved since sacrificing the nerve has only a partial effect upon the latissimus dorsi.
- The specimen is freed from the latissimus dorsi and suspensory ligaments in the axilla, where large veins and lymphatics should be ligated. Hemostasis is ensured and the two major nerves are checked to make sure they are free of ligature and integrity is verified with a gentle pinch that results in a muscle twitch. The wound is irrigated with saline and once again inspected for hemostasis.
- Two closed-system perforated suction catheters are inserted through separate stab wounds made in the lower flap posteriorly. One catheter is directed up to the axilla and the other is secured anterior to the pectoralis major. A few stapes are used to roughly reapproximate the skin edges and then buried interrupted deep dermal sutures are placed, removing the staples as sutures are placed. A barbed Monocryl suture is used in the subcuticular layer. Long SteriStrips are placed on top of the incisions. Fluffed RAY-TECs are placed on top of the incision and an abdominal binder is used as a compressive dressing. The drains are attached to the binder with safety pins.
Postoperative Considerations
- Patient is usually discharged on POD1 with drain education and follow up in clinic in 1 week
- Drains are removed when output is <30 cc/day
- The first week after surgery, the arm is used normally. The second week after surgery, physical therapy exercises are used to ensure return of full range of motion.
Postoperative Complications
- Seroma
- Abscess
- Nerve damage
- Surgical site infection
- Skin flap necrosis
- Chronic pain
- Lymphedema