Gastroschisis was first described in 1547 by Conrad Wolffhart followed by a report by J. Calder in 1733. The term wasn’t coined until 1894, when Cesare Taruffi, an Italian pathologist, utilized the term in his congenital malformations book.
Etiology
- Embryologic
- Risk factors: tobacco, nitrosamine exposure, COX-inhibitors, decongestants
Epidemiology
- Young maternal age
- Low socioeconomic status
- Change in paternity
Pathogenesis
- Embryologic failure of migration of the lateral fold on the right side
- Herniation of midgut into umbilical cord
Presentation
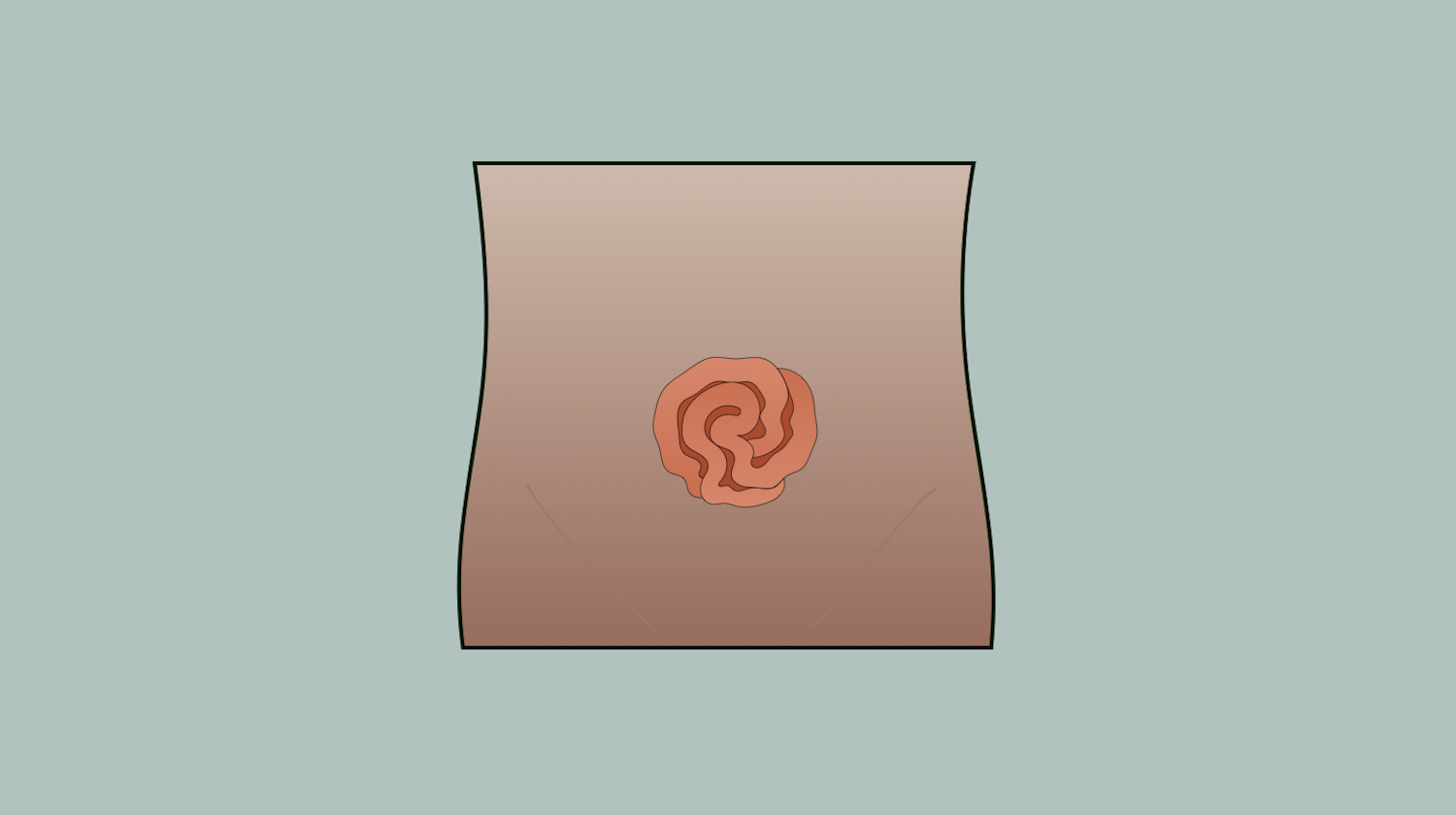
- Defect to the right of an intact umbilical cord, at the side of the obliterated right umbilical vein
- No sac covering the abdominal viscera
- Fascial defect usually 4 cm in diameter
- More common to have intestinal atresia
Labs
- Elevated alpha-fetoprotein
Imaging
- Prenatal ultrasonography
- Most common diagnostic method
- Free-flowing bowel loops in amniotic fluid with associated defect in abdominal wall
Treatment
- Prenatal diagnosis
- Delivery at hospital with NICU and pediatric surgery
- Cesarean or vaginal delivery
- Placement of infant into warm, saline-filled plastic “bowel bag” up to nipple line to minimize heat and fluid losses
- Placement of NG tube
- Broad-spectrum antibiotics x48 hours
- Reduction of eviscerated bowel
- Primary reduction successful 50-80% of the time
- Ringed silo bag is placed if primary reduction is unsuccessful and contents are gradually reduced over several days followed by…
- Operative suture closure of fascia and skin
- Sutureless delayed spontaneous closure at bedside by covering defect with or without umbilical cord followed by watertight clear dressing
- Dressing can then be removed day 4 when intraabdominal contents are adhered
- Dressing changed to dry dressing over cord remnant or Vaseline dressing over exposed bowel
Relevant Information
- Safe intraabdominal pressure is <15 mmHg
Complications
- Postoperative ileus