Melanoma is a form of skin cancer arising from mutated melanocytes, the pigment-producing cells. In 1787, John Hunter performed the first surgical excision of melanoma, despite not knowing what it was. The tumor was preserved in an English museum and later demonstrated to be metastatic melanoma after being reviewed under a microscopy in 1968. René Laennec first identified and described melanoma in 1804 during a lecture given in Paris.
Epidemiology
- Fifth most common cancer in the United States
- Breslow thickness is most important factor in overall survival, nodal, and distal metastatic risk
- Lesions <1 mm thick has 10-year survival of 92%
- Lesions >4 mm thick has 10-year survival of 50%
- Ulceration is a negative prognostic factor
Pathogenesis
- Somatic mutations
- Phenotypic risk factors
- Blue/green eyes
- Fair skin
- Red hair
- Environmental exposure
- Sunburn
- UV radiation
- Genetic mutations: CDKN2A
Presentation
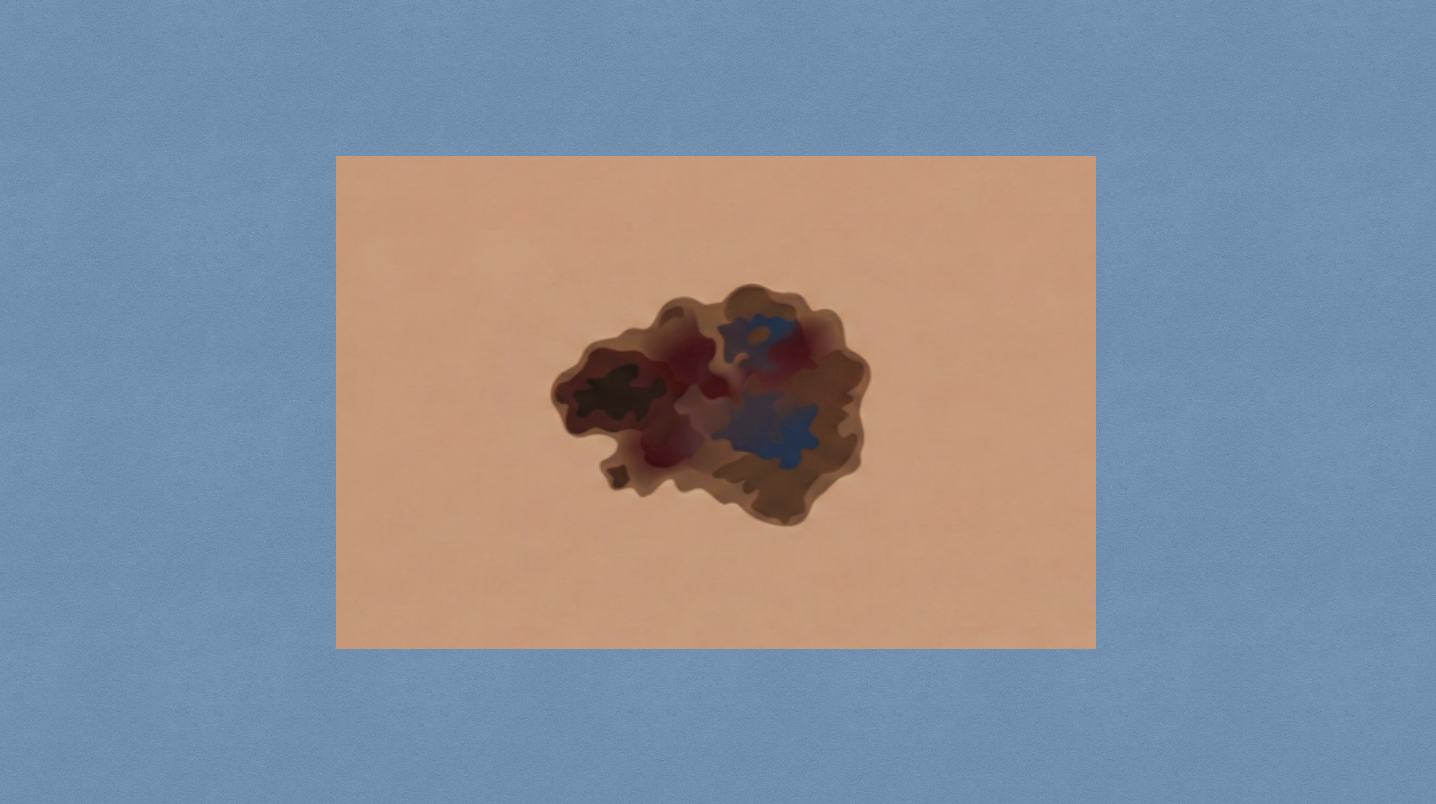
- Evaluate using ABDCDE method
- Asymmetry
- Border irregularity
- Color variegation
- Diameter >6 mm
- Evolving lesion
- Location
- Most common
- Males: back
- Females: legs
- Metastasis
- Most common metastasis: lungs
- Melanoma is most common met to small bowel
- Most common
Workup
- Full-thickness excisional biopsy
- Down to subcutaneous fat
- 1-3 mm margins
- Alternative workup includes either full-thickness punch biopsy or incisional biopsy through the thickest portion of the lesion
- Shave biopsy
- Have been used with increased frequency especially for lesions with low index of suspicion
- Pitfalls include potential inability to reflect Breslow depth, however it allows for rapid, inexpensive information
Staging
- Biopsy results
- Breslow thickness
- Ulceration status
- Nodal basin physical exam
- Imaging, if appropriate
- CT or PET, for patients with advanced (T4b) primary tumor, stage III disease, or symptoms concerning for advanced disease
- Brain MRI, for stage IIIC or above
Subtypes
- In situ
- Hutchinson’s freckle
- Epidermis only
- Lentigo maligna
- Least aggressive subtype
- Superficial spreading
- Most common type
- Radial growth initially, can grow vertically if untreated
- Acral lentiginous
- Palms/soles
- Very aggressive
- Subungal: below fingernail
- Nodular
- Vertical growth first
- Most aggressive
Approach
- Melanoma in situ (stage 0) → local excision with 0.5 cm margins
- Invasive melanoma
- Thickness ≤1 mm → excision with 1 cm margin
- Thickness 1-2 mm → excision with 1-2 cm margin
- Thickness >2 mm → excision with 2 cm margin
- If located on digit or under nail bed, amputation might need to be performed in order to achieve adequate margins
Treatment
- Surgery
- Excision
- Fusiform incision with ratio 3:1 for long:short axis
- Small skin flaps to aid in tension-free closure
- Wound vacuum may help with challenging areas
- Lymph node
- FNA for clinically palpable LNs, with resection if positive
- Sentinel lymph node biopsy (SLNB)
- Indications: ≥T1b (≥0.8 mm or ulcerating)
- Indications for node retrieval
- Dye: all nodes that have taken up dye
- Radiotracer: all nodes with >10% highest ex-vivo count
- Any firm node, regardless of dye/radiotracer
- Completion lymphadenectomy
- Axillary lymph node dissection (ALND)
- Indications: positive SLNB or axillary nodes with no primary
- Include level III nodes for melanoma
- Groin dissection
- Superficial groin (inguinofemoral) dissection
- Indication: positive SLNB
- Femoral triangle borders: sartorius (lateral), adductor longus (medial), inguinal ligament (superior)
- Deep inguinal (iliac-obturator) dissection
- Indications
- Positive Cloquet’s lymph node
- >4 positive LN on superficial dissection
- Enlarged ileo-obturator LNs on preop imaging
- Clinically palpable or extracapsular invasion of femoral LNs
- Indications
- Superficial groin (inguinofemoral) dissection
- Axillary lymph node dissection (ALND)
- Can consider ultrasound observation if the sentinel LN is positive
- Excision
- Systemic therapies
- Immunotherapy
- Nivolumab: monoclonal antibody against PD-1
- Pembrolizumab: monoclonal antibody against PD-1
- Ipilimumab: monoclonal antibody against CTLA-4
- Molecular targeted therapy for BRAF v600-activating mutations
- Dabrafenib (BRAF inhibitor) & Trametinib (MEK inhibitor)
- Vemurafenib (BRAF inhibitor) & Cobimetinib (MEK inhibitor)
- Encorafenib (BRAF inhibitor) & Binimetinib (MEK inhibitor)
- Immunotherapy
- Metastasis
- Limited/resectable → systemic therapy and resect
- Disseminated/unresectable → systemic therapy
Relevant Information
- Pregnancy
- Surgical excision of primary lesion with appropriate margins under local anesthesia
- Ideal to perform in second trimester
- Melanoma by location
- Head and neck melanoma
- Age >70 years old
- Commonly arise in face
- Hand and foot melanoma
- Usually more advanced
- Limited skin mobilization can make for difficult skin closure after excision
- Head and neck melanoma
- Desmoplastic melanoma
- Age >60 years old
- Thick tumor, predominant in head and neck
- Associated with S-100 protein