Acute compartment syndrome occurs when there is an increased pressure within the closed osteofascial compartment which results in impaired circulation within a few hours of the inciting event. Richard von Volkmann, a German surgeon, was the first person to describe compartment syndrome and did so in 1881.
Etiology
- Ischemia
- Trauma
- Crush injuries
- Severely comminuted or segmental fractures → tibial fractures (most common)
- Widely displaced joint or fracture pieces
- High-energy injuries with impaired sensation
- Burn injuries
- Tight dressing or cast
Pathogenesis
- Inciting event (i.e., ischemia, trauma, burn injury) occurs and causes a decreased intracompartmental space and increased intracompartmental fluid volume due to the inability of the fascia to expand
- No equilibrium between venous outflow and arterial inflow is permitted
- Venous pressure and venous capillary pressure increases which leads to the intracompartmental pressure to increase
- Decreased oxygenation of tissues occurs as a result of decreased arterial inflow and venous outflow, leading to ischemia
- Usually manifests within a few hours, but can be up to 48 hours later
History
- Tense, tender leg muscles
- Leg numbness
- Dysesthesias
Physical Exam
- Tense, tender muscles → “wood-like” feeling
- Pain on passive motion (early)
- Impaired motor function
- Pain out of proportion
- Intracompartmental pressure > 30 mmHg (normal pressure is < 10 mmHg)
- Pulses may be present! Presence or absence of a pulse isn’t definitive.
- 5Ps: pain, pulselessness, paresthesia, paralysis, pallor
Labs
- CPK (creatinine phosphokinase): may be elevated; suggestive of muscle breakdown from ischemia, damage, or rhabdomyolysis
Imaging
- Radiograph if fracture is present
- Intracompartmental pressure
- Delta pressure: difference between diastolic blood pressure and intracompartmental pressure
Treatment
- Surgical emergency!
- Flow restoration
- Thrombectomy
- Embolectomy
- Bypass
- Thrombolytic therapy
- Lower extremity fasciotomy
- If intra-compartmental pressure is > 30 mmHg
Relevant Information
- Fascia
- Thin, inelastic connective tissue
- Surrounds muscle compartments and has a limited capacity for expansion
- Compartment syndrome is most likely to occur in the lower extremity, likely as a result of ischemia or restoration of flow after a period of ischemia
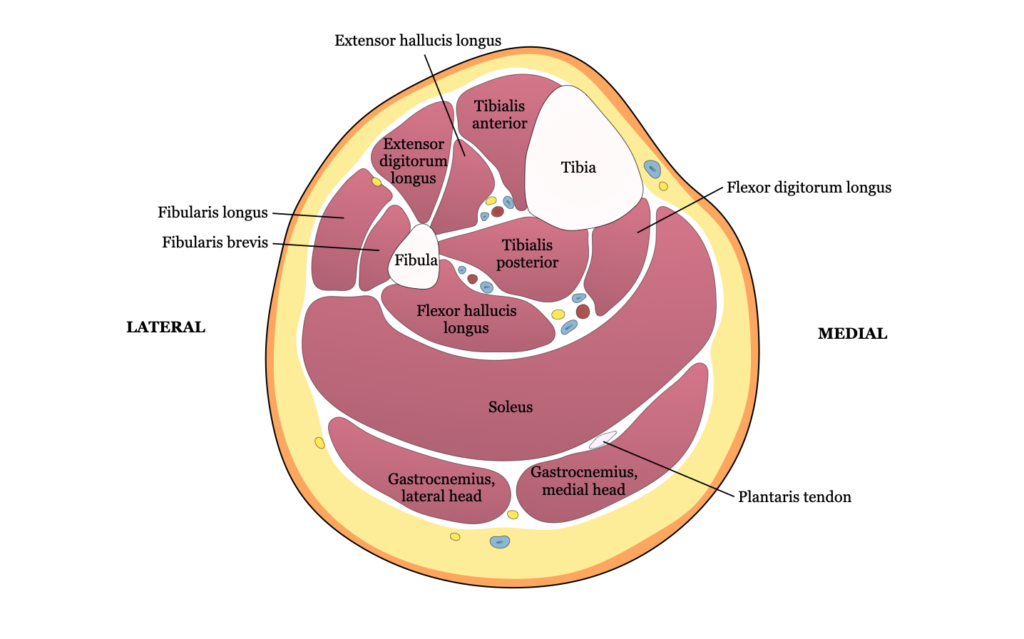
- Superficial branch of the peroneal nerve: lies adjacent to the intermuscular septum between anterior and lateral compartments
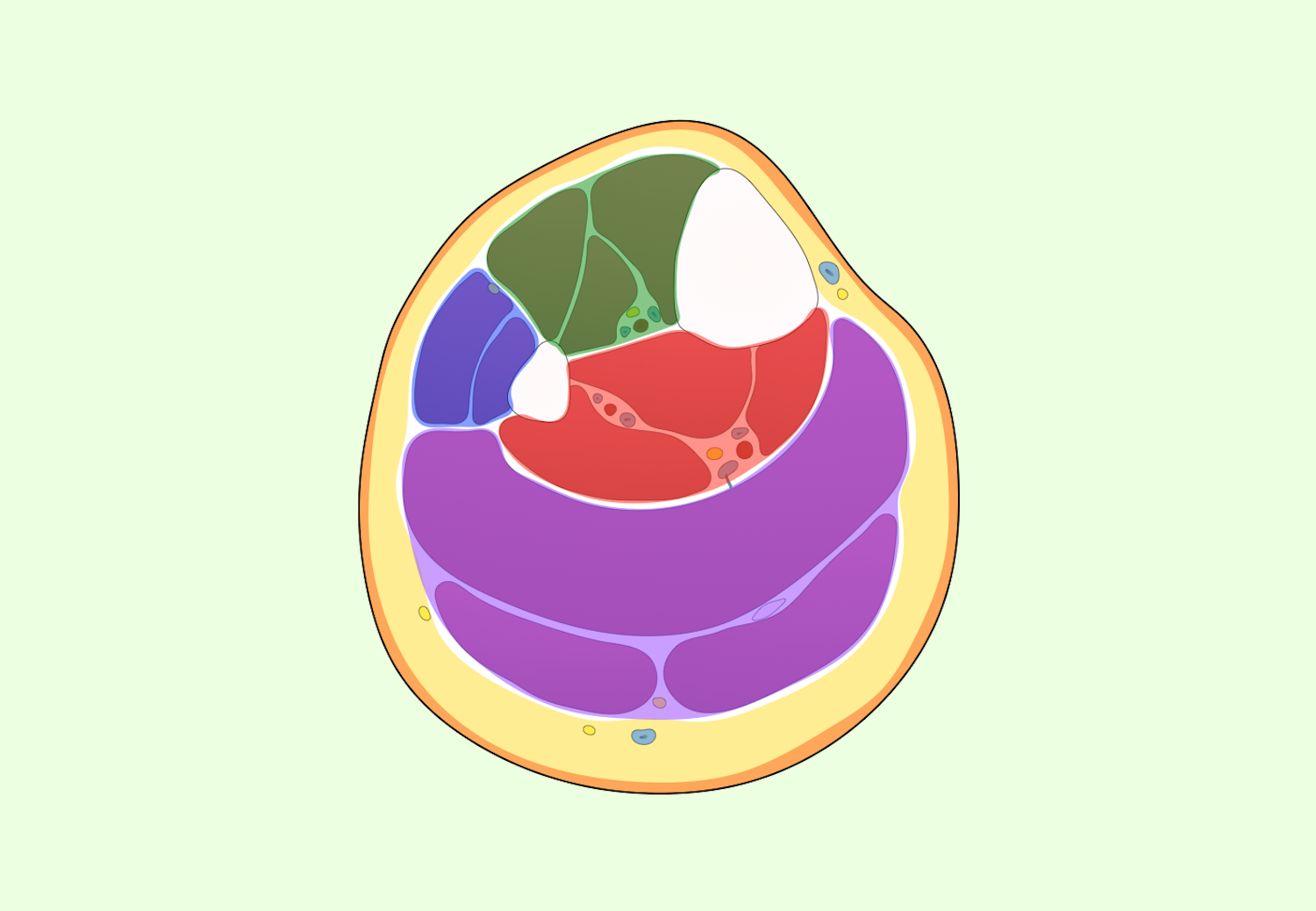
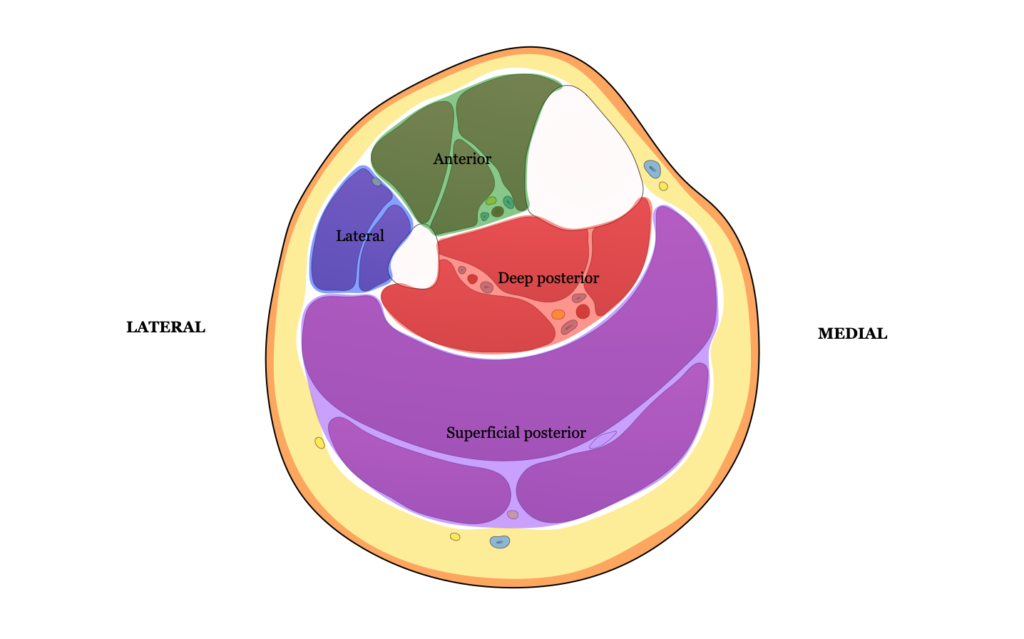
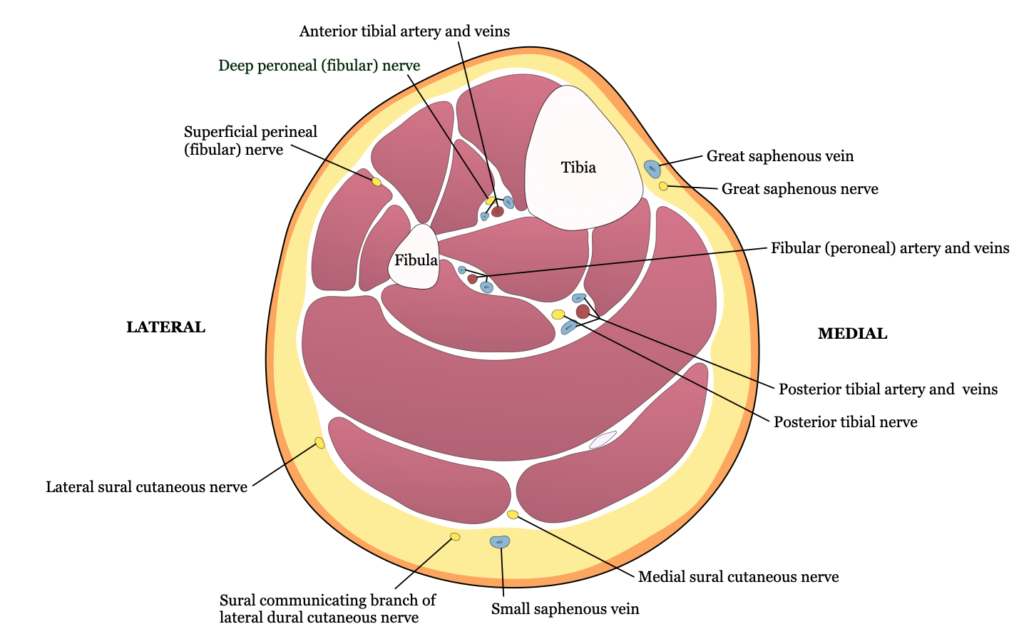
- Compartments of the leg
- Anterior → most common location for compartment syndrome
- Tibialis anterior
- Peroneus tertius
- Extensor hallucis longus
- Extensor digitorum longus
- Lateral
- Peroneus longus
- Peroneus tertius
- Superficial posterior
- Gastrocnemius
- Soleus
- Plantaris
- Deep posterior
- Tibialis posterior
- Popliteus
- Flexor hallucis longus
- Flexor digitorum longus
- Anterior → most common location for compartment syndrome
Complications
- Contractures
- Pain
- Rhabdomyolysis
- Nerve damage, associated numbness/weakness
- Infection
- Renal failure
- Death
Differential Diagnoses
- Deep vein thrombosis
- Cellulitis
- Gas gangrene
- Rhabdomyolysis
- Peripheral vascular injuries