Appendectomy is the surgical removal of the appendix. The first planned appendectomy was done by Lawson Tait, a British gynecologist, in May 1880. Claudius Amyand had previously removed the appendix in 1735, but it was not a planned, intentional procedure. Prior to the routine use of appendectomy, appendicitis and appendiceal abscesses were treated with drainage. In 1759, Mestivier diagnosed an appendiceal abscess and drained a pint of pus. Despite this, his patient died. William Parker successfully drained an appendiceal abscess in 1843 and saved his patient’s life.
Indications
- Acute appendicitis
- Peri-appendiceal abscess
- Appendiceal neoplasms
Preoperative Considerations
- IVF, as indicated
- Broad-spectrum IV antibiotics (against Gram-negative and anaerobics)
Risks
- Infection
- Abscess
- Stump appendicitis
- Death
Relevant Anatomy
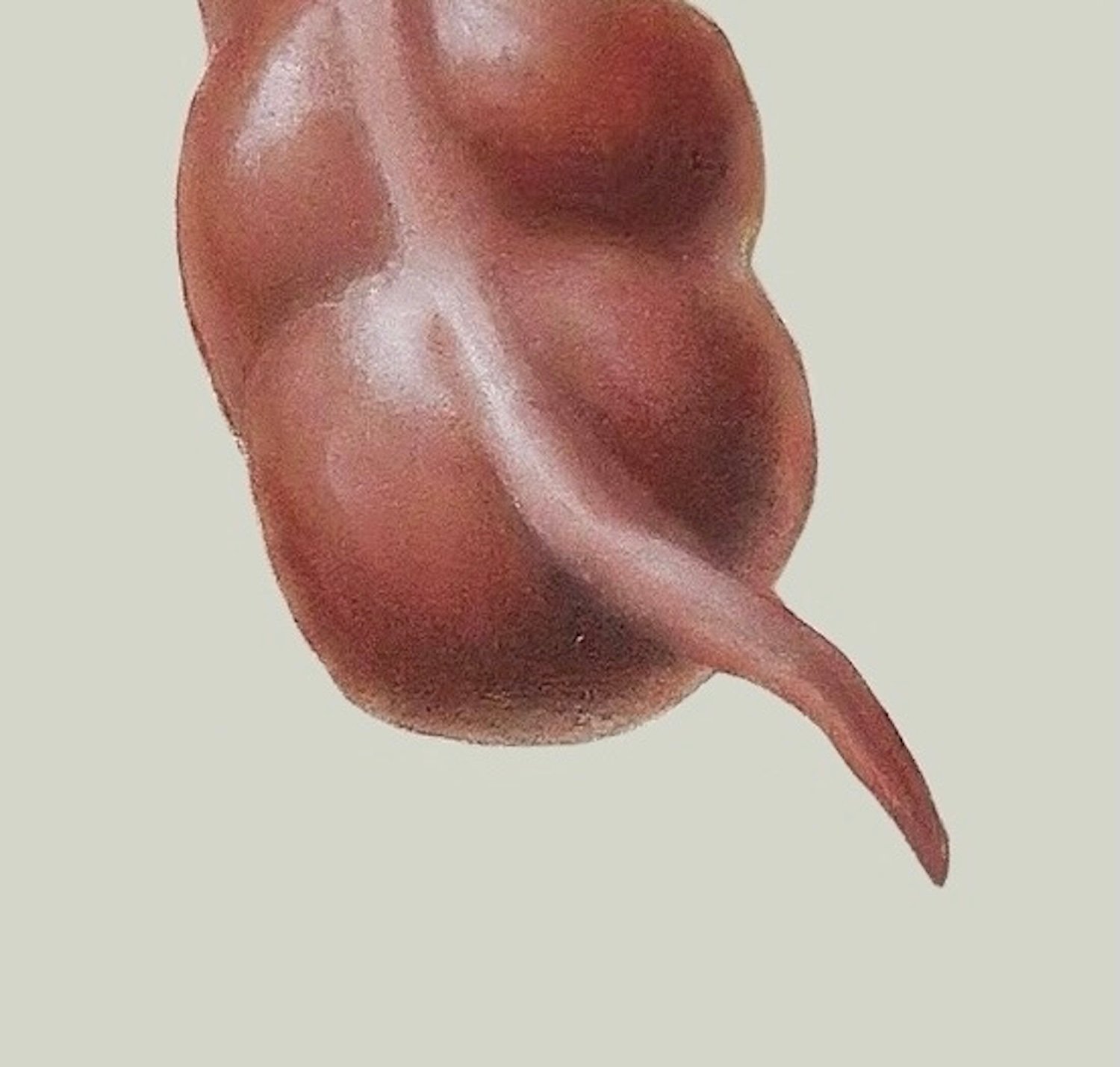
- Base of the appendix arises from convergence of taenia coli. It is attached to the terminal ileum by the mesoappendix, a triangular fold of mesentery that is also connected to the cecum.
- Usually 8-10 cm long
- Vestigial (rudimentary) organ: organs, tissues or cells in a body which are no more functional the way they were in their ancestral form of the trait
- Supplied by appendicular artery, arises from ileocolic artery 35% of pts
- Types of incisions for open appendectomy
- McArthur-McBurney: oblique muscle-splitting incision
- Rockey-Davis: transverse incision
- Midline incision
- Appendix orientation
- Retrocecal (65%)
- Pelvic (31%)
- Subcecal (2.3%)
- Preileal (1.0%)
- Retroileal (0.4%)
- Fold of Treves
- Bloodless fold; no sizable blood vessels
- Peritoneal structure that extends from the antimesenteric border of the terminal ileum to the base of the appendix, or anterior surface of the mesoappendix, or both
- Can aid in the recognition of the ileocecal region and base of the appendix
Surgical Technique
- Patient is placed in supine position and prepped and draped in the usual sterile fashion. The access port is placed (some surgeons use umbilical port, while others prefer LLQ, lower midline, or RUQ) and the abdomen is insufflated with CO2.
- The camera is inserted and set up and visualization of all quadrants is performed with findings noted. Two additional 5-mm ports are placed – one in the LLQ lateral to the rectus (to avoid epigastric vessels) and through the midline linea alba in a suprapubic position (to avoid the bladder). Placing ports in a triangular pattern such as this, with a hand’s breadth between each port, is helpful as the three instruments in each port compete for space to maneuver.
- Patient is placed in Trendelenburg position with the right side elevated to hold the small bowel away from the RLQ.
- If a normal appendix is found, another inflammatory process is searched for. Potential sources: tubo-ovarian diseases, inflammatory bowel disease, Meckel’s diverticulitis
- Once the diagnosis of appendicitis is made, the appendix is mobilized.
- Appendix position varies. Safe opening of any peritoneal covering or equivalent of the lateral line of Toldt along the cecum may require an additional port.
- Laparoscopic removal begins with splaying out the mesoappendix using grasping forceps on the mesentery. The appendix is NOT grasped, as it could cause rupture of the appendix. The mesentery is opened at the base of the appendix and the mesoappendix is divided in one or more transections using an endoscopic vascular stapling instrument. The base of the appendix is divided with the endoscopic cutting linear stapler.
- Removal of a small, minimally inflamed appendix can be removed through the shaft of a 10-mm port. A bag may be used for removing an enlarged or suppurative appendix. The appendiceal stump and stapled mesoappendix are inspected for hemostasis. Removal of 5-mm ports is done under direct visualization.
- The abdomen is decompressed and the fascia of the 10-mm port is closed. Port sites are closed with glue.