Lumpectomy is the removal of a breast tumor while preserving the normal surrounding healthy tissue. Mastectomy is the removal of all glandular breast tissue.
Discussion of Surgical Options
- Early-stage breast cancer (stage I and II) usually managed with primary surgery (breast-conserving or mastectomy)
- Neoadjuvant therapy common indications
- HER2-positive breast cancer
- Triple-negative breast cancer
- When downstaging of of disease in breast and/or axilla is desired
- Genetics
- About 10% of newly diagnosed breast cancers are due to strong family history or genetic predisposition
- Oncotype DX
- Analyzes 21 genes to predict recurrence risk and determine which patients will benefit from chemotherapy
- Indicated for ER+, HER2- tumors that are either stage I, II, or IIIa
- Randomized prospective trials have demonstrated similar breast cancer-specific and overall survival when comparing lumpectomy plus radiation versus mastectomy
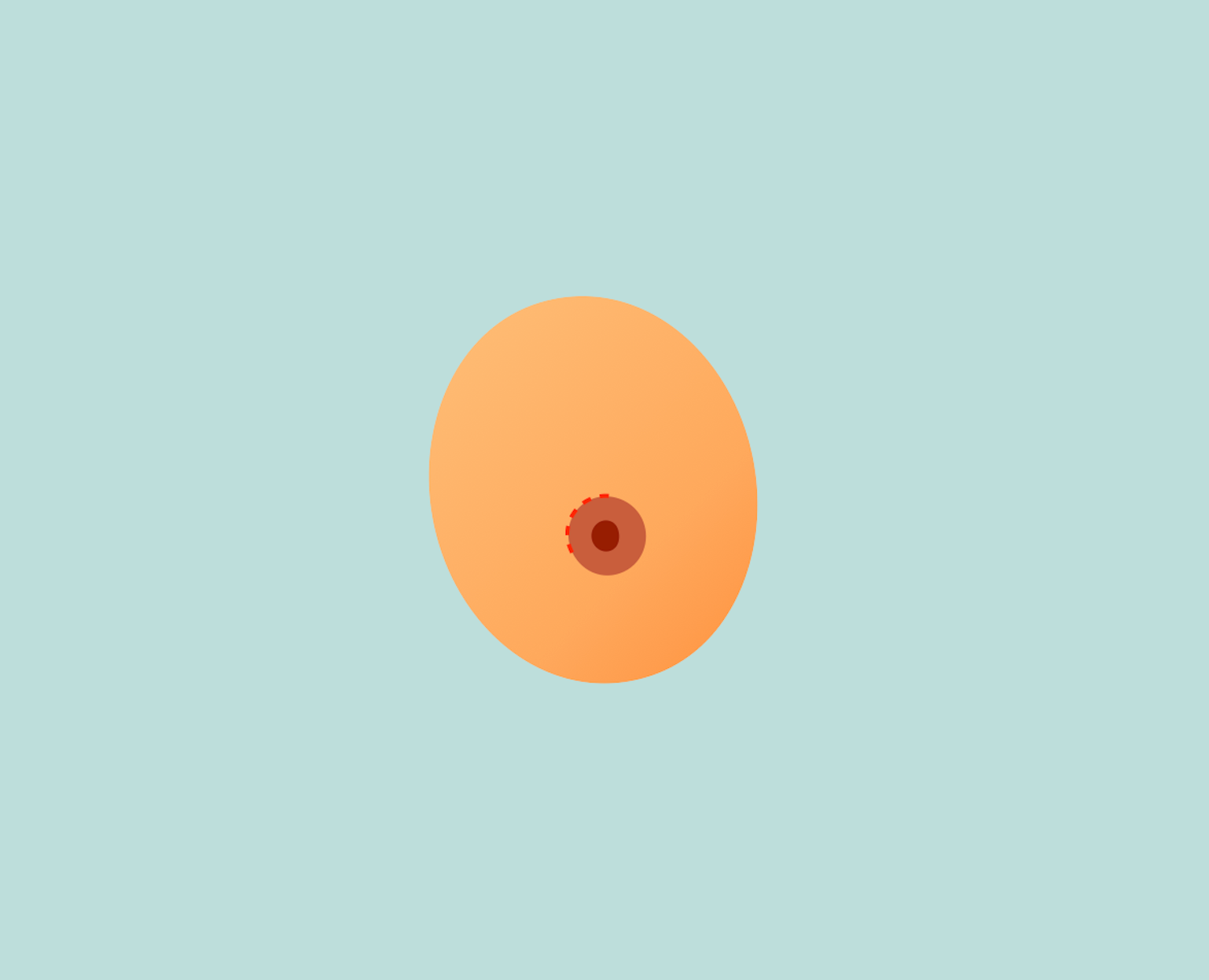
Lumpectomy
- Preserves the cosmetic effect of the breast
- Whole-breast radiation is an essential component of breast-conserving therapy and serves to decrease the risk of breast cancer recurrence
- Contraindications
- Current pregnancy (due to radiation)
- Prior radiation therapy, including chest radiation
- Multicentric or widespread disease
- Large tumor size in relation to breast (compromising cosmesis)
- Active connective tissue disease
- Incision planning
- Periareolar incision can be used in select patients
- When periareolar incision is not feasible, incisions should follow natural skin creases (Langer’s lines)
- Margins
- Invasive cancer → no tumor at inked surface
- DCIS → 2 mm margins
- Reexcision is necessary if pathology comes back with positive margins. The number of reexcisions that can be attempted varies depending on the volume of breast tissue that was previously resected in relation to the size of the breast. Failure to achieve clear/negative margins may warrant conversion to completion mastectomy.
Mastectomy
- Types of mastectomy
- Simple mastectomy without reconstruction
- Large elliptical incision is made encompassing the nipple-areolar complex
- Resect enough skin so there is minimal redundant skin with flat closure
- No need for axillary surgery
- Modified radical mastectomy
- Indications → biopsy-proven positive lymph node involvement
- Includes concurrent level I and level II axillary lymph node dissection
- Performed along the plane defined by suspensory ligaments of Cooper
- Thickness of mastectomy flap varies according to thickness of subcutaneous tissue in the individual
- Skin sparing or nipple-sparing mastectomy can be considered for patients considering mastectomy with reconstruction
- Skin-sparing mastectomy
- Removal of all glandular breast tissue and nipple-areolar complex but preserves as much of the skin to allow for reconstruction
- Elliptical incision made incorporating the nipple-areolar complex. The incision can be planned with the plastic surgeon who will be performing the immediate reconstruction.
- Nipple-sparing mastectomy
- Preserves entire skin envelope of breast including nipple-areolar complex
- Contraindications
- Locally advanced breast cancer
- Extensive disease in periphery of breast
- Direct invasion of the nipple with cancer
- Tumors ≤1 cm from the nipple
- Avoided in patients with prior history of radiation, smoking history, and larger or ptotic breasts (due to increased risk of flap/skin necrosis)
- Incision
- Inframammary fold is most common
- Inferolateral allows for access to axillary tail if lymph node sampling/dissection is needed
- Radial
- Periareolar incision
- Closed suction drains beneath the mastectomy flaps and the axilla is standard practice in order to prevent seroma formation
- Simple mastectomy without reconstruction
- Indications
- Patients with contraindications for breast-conserving surgery
- Inflammatory breast cancer
- Patients that prefer mastectomy
- Bilateral prophylactic mastectomy reduces risk of developing cancer by >90% in patients with BRCA mutation
- Complications
- Hematoma
- Seroma
- Wound infection
- Skin flap necrosis
- Chronic pain
- Phantom breast syndrome
- Arm morbidity
- Bleeding (occurs 3% of the time)
Axilla Management
- Axillary lymph nodes receive 85% of lymphatic drainage from the breast and serves as area where metastatic breast cancer cells are most likely to be found
- Sentinel lymph node biopsy
- Developed in 1994
- Allowed for omission of axillary lymph node dissection in most patients with clinically node-negative disease
- Provides prognostic information useful for decisions regarding adjuvant therapy
- Can be performed in conjunction with lumpectomy or mastectomy
- Relevant trials → AMAROS (After Mapping of the Axilla: Radiotherapy or Surgery)
- Axillary lymph node dissection
- Indications
- Clinically positive axillary lymph nodes confirmed by fine-needle aspiration or core needle biopsy
- Locally advanced breast cancer
- Inflammatory breast cancer
- Generally involves removing level I and II lymph nodes
- Level III lymph nodes may be removed if there are grossly positive level I or II lymph nodes intraoperatively
- Neoadjuvant therapy may be considered in patients with clinically positive lymph nodes in order to downstage the axilla
- Complications: lymphedema
- Indications