The first escharotomy was recorded in 1607 by a German surgeon. However, it wasn’t until the 1950s that the procedure gained more popularity. This was when surgeons like Blocker and Moyer utilized the procedure to relieve vascular compromise in burn patients.
Etiology
- Involves partial or full-thickness skin destruction
- Causes include fire (most common), hot liquid, or solids (least common)
- Risk factors: male (68%), 20-30 year olds as well as infants and elderly
Physical Exam
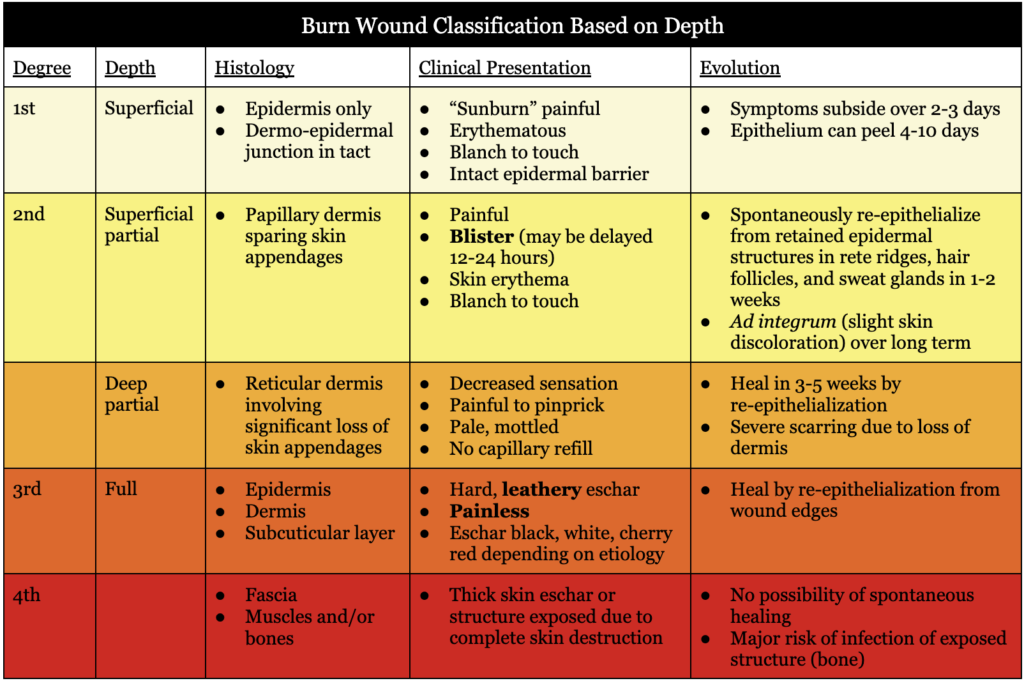
- Burn depth
- Depends on temperature and time/length of exposure
- Initial clinical evaluation is only 64-76% accurate – depth evolves first 24-48 hours
- External factors: wound care, fluid administration, external temperature
- Burn size
- Quantified based on TBSA affected by second- and third-degree burns
- Adults: rule of nines
- Head, chest, abdomen, upper back, lower back, right arm, left arm, right upper leg, right lower leg, left upper leg, left lower leg
- Add 1% for perineum
- ~1% per palmar area
- Children/infants: Berkow formula, Lund table, Browder table
- Rough estimation by equating patient’s open hand with 1% TBSA and transposing the measurement visually onto the wound to determine wound size
- Most accurate assessment is with digital imaging
- Adults: rule of nines
- Quantified based on TBSA affected by second- and third-degree burns
- Location
- Areas requiring specific consideration: ophthalmologic, genital, feet, hand, facial
- Corneal injury should be suspected in facial burns
- Facial and cervical burns may require intubation (airway swelling concern)
- Inhalation injuries
- Injury of upper airway (above larynx) usually caused by heat
- Suspected in causes of facial burns, singed nose hairs, signs of swelling, erythema, stridor, hoarseness
- Injuries of lower respiratory tract (below larynx) usually caused by chemical
- Suspected in cass of carbonaceous sputum, elevated carboxyhemoglobin level >10%, stridor, hoarseness, tachypnea
- Diagnosed based on bronchoscopy
- Injury of upper airway (above larynx) usually caused by heat
- Genital and perineal burns may require diversion by Foley catheter and/or fecal diversion
- Compartment syndrome
- Generalized edema under an eschar can cause increased interstitial pressure and compress circulation leading to severe tissue damage
Severe Burn Injuries
- >10% total body surface area (TBSA) in elderly patients
- >20% TBSA in adults
- >30% TBSA in children
- Classification based on larger studies indicating risk of adverse outcomes dependent on burn size
Burn Workup Phases
- Phase I → Emergency Management (0-6 hours)
- First aid care and triage to burn center
- Primary traumatic survey (ABCs)
- Secondary survey
- Begin resuscitation
- Urgent surgical care: escharotomy, fasciotomy
- Simple wound care antiseptic dressing
- Phase II → Stabilize Patient (major burns)
- Treat burn shock
- Fluid resuscitation and organ failure support
- Phase III → Burn Wound Coverage
- Surgical debridement wound coverage
- Optimize condition (nutrition support)
- Treat complications
- Phase IV → Rehabilitation
- Prevent retraction and contracture
Treatment
- Burns not healed by 14 days after burn injury will most likely require surgical intervention; they are unlikely to heal
- Fluid replacement
- Formulas
- Parkland formula
- Initial fluid for first 24 hours if >20% BSA
- Total fluid = BSA x weight (kg) x 4 cc/kg/BSA
- BSA used is a whole number (25% = 25)
- Burns ≥2nd degree (1st degree doesn’t count)
- Give first half over 8 hours, second half over 16 hours
- Modified Brooke formula
- Same as Parkland formula, but uses 2 cc/kg/BSA instead of 4 cc/kg/BSA
- Minimizes risk over resuscitation
- Parkland formula
- Pediatrics → use 3-4 cc/kg/BSA
- Use lactated ringers for first 24 hours
- Formulas
- Management
- Airway, breathing, circulation
- Definitive treatment
- Superficial: salves/ointment
- Superficial partial: clean, dressing
- Deep partial or full thickness: debride, skin graft at 24-48 hours
- Defer face, genitals, palms, and soles for the first week
- St hands in extension
- Antibiotics
- Topicals
- Bacitracin and Neomycin
- Poor Gram negative coverage
- Painless
- Side effects: nephrotoxicity
- Silver sulfadiazine (Silvadine)
- Most commonly used in partial thickness
- Effective for Candida
- Painless
- Side effects: neutropenia, thrombocytopenia
- Mafenide acetate (Sulfamylon)
- Carbonic anhydrase inhibitor
- Good eschar penetration
- Broadest spectrum for Pseudomonas and Gram negative rod
- Side effects: metabolic acidosis
- Silver nitrate
- Side effects: electrolyte imbalance (Na, Cl, K)
- Mupricin
- Best for MRSA
- Bacitracin and Neomycin
- Systemic agents are not for prophylaxis but instead if diagnosed with an infection
- Topicals
- Escharotomy
- Performed at bedside
- Extremity → vertical incisions
- Torso
- Chest and abdomen → transverse incisions
- Anterior axillary lines → vertical incisions
- Incision of the eschar is the only thing required in order to spare fascia
Admission Criteria
- 2nd degree burns
- Age <10: >10% BSA
- Age 10-50: >20% BSA
- Age >50: >10% BSA
- Any to face, hands, feet, perineum, or major joints
- 3rd degree burns: >5% BSA
- Other factors
- Any electrical or chemical burns
- Any concomitant inhalation injury or multiple trauma