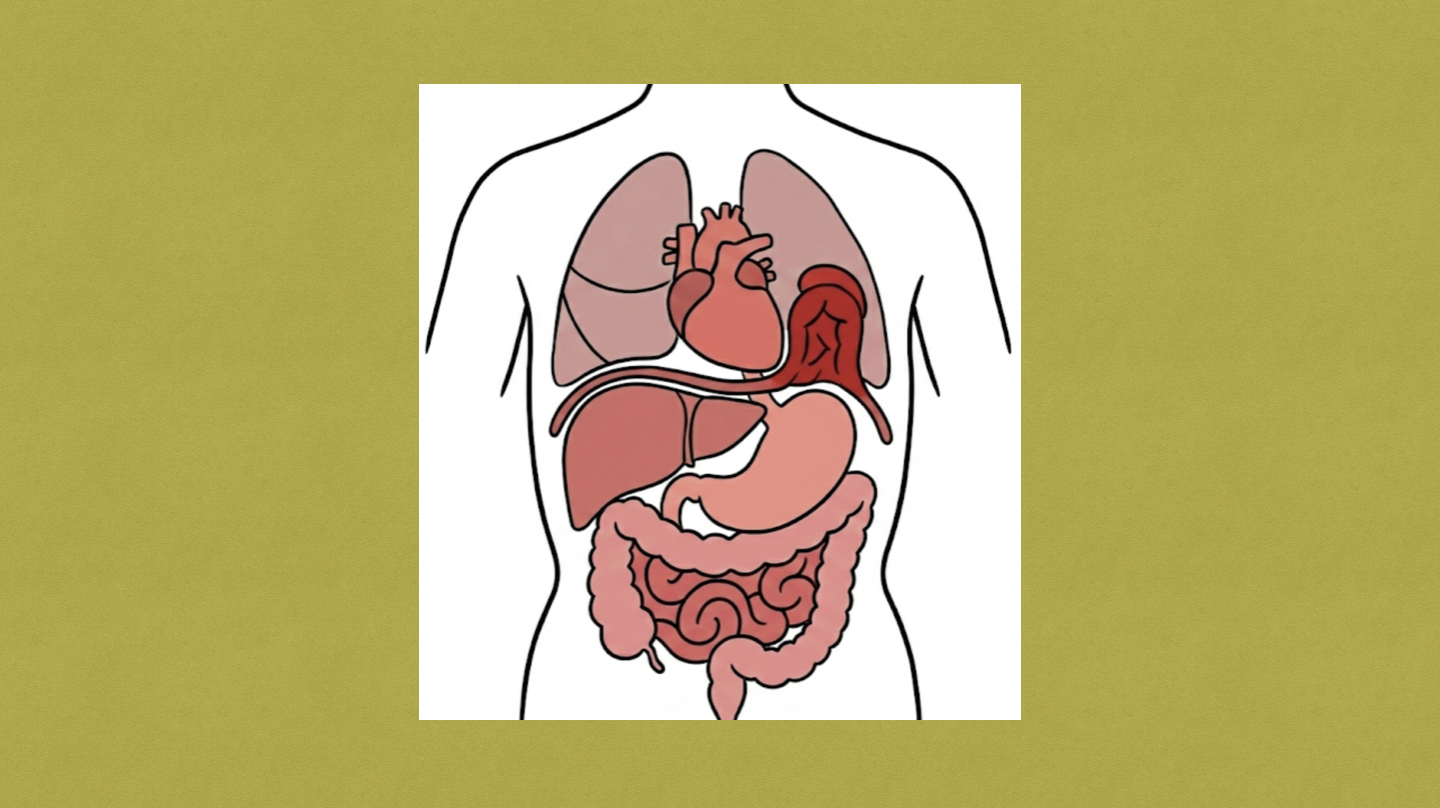
Congenital diaphragmatic hernia (CDH) occurs when there is improper development of the diaphragm which results in herniation of the abdominal contents into the thorax. Vincenz Alexander Bochdalek described the common posterolateral defect in 1848 and is the reason why these hernias are referred to as “Bochdalek hernias.” In 1905, Lothar Heidenhain published the first successful repair in which a midline laparotomy incision was made to reduce the herniated contents back into the abdomen on a 9-year-old boy.
Pathogenesis
- Thought to be due to impaired development of pleuroperitoneal fold or development of posthepatic mesenchymal plate
- Potential theories include
- Environmental exposure (e.g., Nitrofen)
- Genetics
- Specific transcription factors: GATA4, ZFPM2, NR2F2, WT1
- Syndromes:
- Fryn syndrome
- Pallister-Killian
- Cornelia de Lange syndrome
- Wolf-Hirschhorn syndrome
- Note
- Diaphragm develops between weeks 7-12 gestation
- Lung develops buds at 6 weeks and branches at around 8 weeks gestation
Presentation
- Most (60-80%) are diagnosed during route prenatal ultrasound
- Respiratory distress, increased work of breathing, tachypnea, accessory muscle use, cyanosis
- Decreased breath sounds or borborygmus (ipsilateral chest)
- Mediastinal shift to contralateral chest
- Asymmetric thorax (ipsilateral more distended)
- Scaphoid abdomen
Management
- Risk stratification is paramount for counseling, intervention, and optimization. This includes evaluating lung size, cardiac anatomy, liver position, and other anomalies which may be present.
- Prenatal ultrasound, MRI, echo
- ABG, serum lactate
- Chromosomal analysis
Imaging
- CXR: confirming diagnosis and identify degree of mediastinal shift
- Echo: identifies pulmonary hypertension and degree of cardiac dysfunction
Treatment
- Fetoscopic endoluminal tracheal occlusion is possible however patients must meet very specific guidelines. This page will focus on neonatal management of congenital diaphragmatic hernias.
- Intubation
- Pressure-limited, permissive hypercapnia, avoid barotrauma
- Ventilator settings
- Initiate FiO2 with saturation goal 80-95%
- Peak inspiratory pressure (PIP): 20-26 cm H2O
- Positive end-expirator pressure (PEEP): 5 cm H2O
- Respiratory rate (RR): 30-40 breaths/minute
- Conventional mechanical ventilation (CMV) is often the mode used initially, however high-frequency oscillatory ventilation (HFOV) is also an option
- Gastric decompression → minimize intestinal distention and improve intrathoracic pressure
- Extracorporeal life support (ECLS)
- Used in 30% of patients with CDH by allowing for cardiopulmonary recovery by providing oxygenation and ventilation along with mechanical support of the heart. How long patients are on ECLS is guided by clinical assessment and therapy can continue for 4-5 weeks.
- Indications
- Hypoxemic respiratory failure on CMV or HFOV
- Hypoxia <80-85%
- Inadequate oxygenation with metabolic acidosis (lactate >5 mmol/L or pH <7.20)
- Hypercarbia (PaCO2 >70 mmHg) with respiratory acidosis (pH <7.20)
- Hypotension resistant to IV fluids and ionotropic support with poor tissue perfusion (UOP <0.5 mL/kg/hr)
- Relative contraindications
- Significant congenital anomalies
- Lethal chromosomal anomalies
- High-grade intracranial hemorrhage
- Weight <1.8 kg (3.97 lb)
- Gestational age <32 weeks
- Timing of repair
- Dependent on multiple factors
- Early repair on ECLS → 24-48 hours
- ***Identified as superior to other two approaches
- Delayed repair on ECLS → 2-3 weeks or when close to decannulating
- Repair after weaning off ECLS
- Surgical approach
- Open repair via left subcostal incision (for LEFT CDH) → note, RIGHT CDH is approached via right subcostal incision
- Explore abdomen and reduce herniated contents
- Repair → must be tension-free
- Primary
- 2-0 Ethibond or silk suture (pledgets recommended for better security)
- Suture placed <1 cm apart in simple interrupted or horizontal mattress
- Patch
- PTFE synthetic patch
- Autologous rotational muscle flap
- Primary
- Thoracoscopic approach
- Resect hernia
- Repair
- Primary
- 2-0 Ethibond or silk suture with intracorporeal knot-tying
- Placed medial to lateral to optimize diaphragm approximation
- The most lateral suture may include the rib/fascia of lower abdominal wall to help strengthen the repair as this area is the most susceptible area to tearing from tying suture
- Patch
- Gore-Tex cut to size and introduced through trocar
- Patch secured to diaphragm using 2-0 Ethibond or silk suture sewing the patch in circumferentially
- Primary
- Open repair via left subcostal incision (for LEFT CDH) → note, RIGHT CDH is approached via right subcostal incision
CDH Staging System
- Defect A
- Smallest defect
- Usually “intramuscular” with >90% hemidiaphragm present
- Involves <10% of circumference of chest wall
- Defect B
- 50-75% hemidiaphragm present
- Involves <50% of circumference of chest wall
- Defect C
- <50% hemidiaphragm present
- Involves >50% of circumference of chest wall
- Defect D
- Largest defect
- Complete/near complete absence of diaphragm
- <10% hemidiaphragm present
- Involves >90% of circumference of chest wall
- Absent posterior rim and miniscule anterior/anterior-medial rim
- Requires patch or muscle flap repair
- No defect diagrams have been created for right-sided defects, so the above descriptions are used and reversed to describe these defects.
- Congenital Diaphragmatic Hernia Staging System PDF
Relevant Information
- Mortality 25-30%
- Complications of CDH
- Cardiac dysfunction
- Pulmonary hypertension: sustained pulmonary arterial pressure leading to inadequate oxygenation and ventilation
- Pulmonary hypoplasia: underdeveloped lungs leading to impaired gas exchange
Complications
- Intraoperative
- Hemorrhage
- Hollow viscous injury
- Ascites
- Hypercarbia
- Postoperative
- Chylothorax
- Abdominal compartment syndrome
- Infection
- Recurrence (2-3%)
Resources
- Canadian Congenital Diaphragmatic Hernia Collaborative (2023 update)
- Congenital Diaphragmatic Hernia Study Group (CDHSG)
- American Academy of Pediatrics Postdischarge Follow-up Report (2026)
- Congenital Diaphragmatic Hernia Staging System PDF