Gastrostomy tubes are placed through the skin into the stomach in order for patients to receive feeds and medications they are unable to obtain through the oral route, which can be for a myriad of reasons. Aristide Auguste Stanislas Verneuil is often credited with the first successful feeding tube placement in 1876. In 1894, Martin Stamm created a different method for creating gastrostomies. The first percutaneous endoscopic gastrostomy tube was introduced in 1979 by the American pediatric surgeon Michael Gauderer and endoscopist Jeffrey Ponsky.
Indications
- Dysphagia
- Altered head/neck anatomy
- Altered mental status
- Inability to meet nutritional needs (e.g., atresia, achalasia, malignancy, anorexia, burns, cancer)
Contraindications
- Esophageal cancer (due to eventual construction of gastric conduit)
- Hemodynamic instability
Preoperative Considerations
- Abdominal wall anatomy
- Abdominal scars
- Abdominal wall thickness
- Expected duration of need for gastrostomy tube
Relevant Information
- Typically left in place for a minimum of 8 weeks
- Preoperative considerations
- Preoperative antibiotics given 30 minutes prior to skin incision
- Antiseptic mouthwash used prior to start of procedure
- Abdominal wall shouldn’t be compression between the bumper and bolster as this can cause tissue necrosis and additional complications
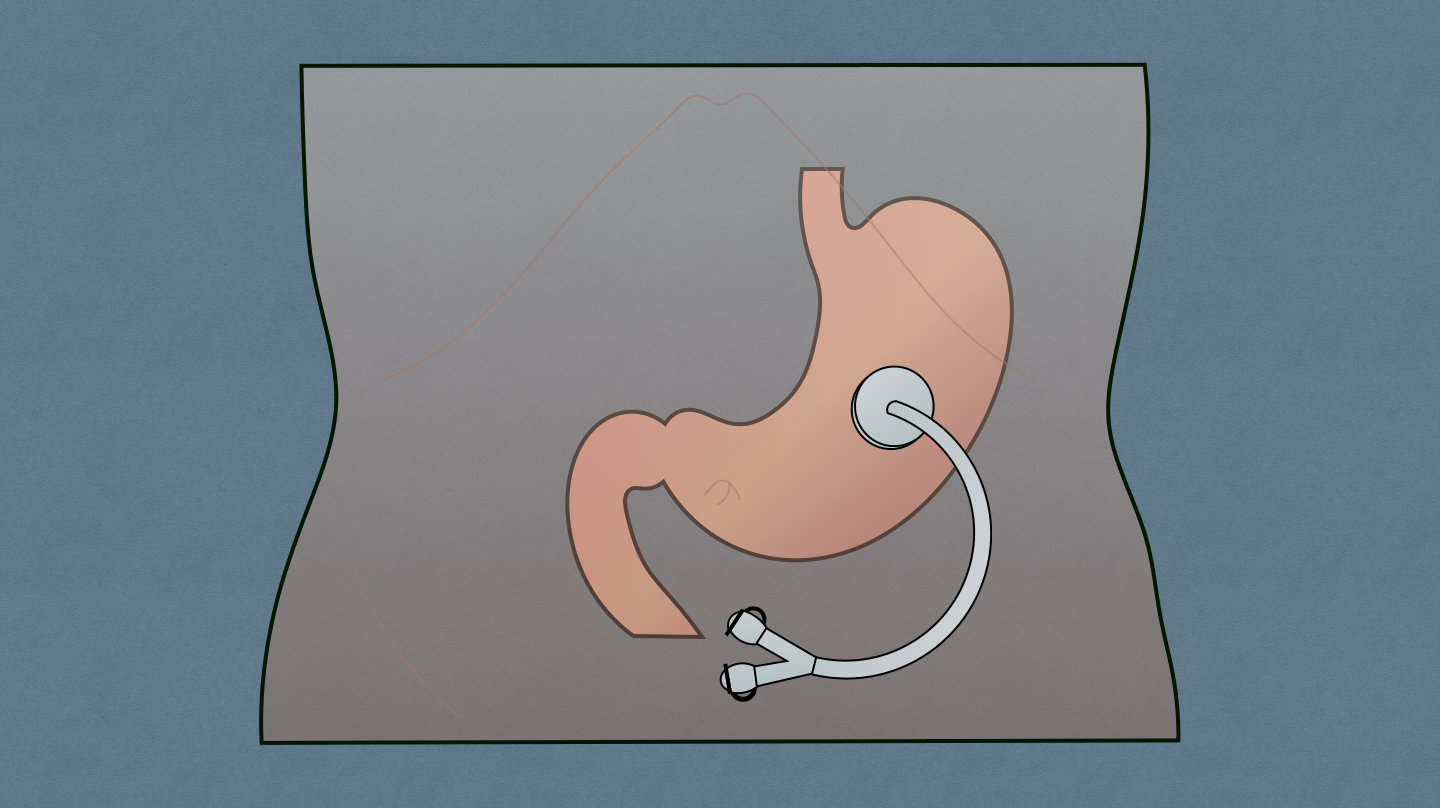
Percutaneous Endoscopic Gastrostomy (PEG) Tube
- Transillumination. The endoscopist advances to the patient’s stomach and insufflates with gas, advancing the scope and directing the light towards the anterior gastric wall of the stomach, 2-3 cm distal to the gastroesophageal junction (GEJ). Room lights are dimmed to ease with visualization of endoscope light. Abdomen is palpated by the surgeon to confirm the correct location, ensuring it is at least 2-3 cm inferior to the costal margin, and then marked and local anesthetic is injected into the skin.
- Needle Localization. A 10-cc syringe is filled with saline and attached to a small gauge needle and advanced perpendicularly through the marked site while drawing back on the needle. If bubbles are visualized in the syringe prior to seeing the needle via endoscopy, then there is concern the needle is in the colon. If bubbles are visualized in the syringe at the same time as the needle is seen via endoscopy, then the position is safely in the stomach.
- Tube Placement. An 11-blade is used to make a small (0.5 cm) skin incision at the selected site. The polypectomy snare prepared by the endoscopist is advanced with its loop centered over the area of mucosa identified during site selection and the needle with the angiocath is advanced through the abdominal wall incision into the stomach and through the snare loop. The needle is then withdrawn, leaving the angiocath in place. The wire is advanced through the angiocath, the snare is tightened, and the endoscope is withdrawn completely. This pulls more of the wire into the stomach, through the esophagus, and out through the mouth.
- Pull Technique. Looped wire that comes out through the mouth is closed over the external portion of the PEG tube and the surgeon pulls the portion of the wire exiting the abdominal wall in order to advance the PEG tube back down into the stomach while the endoscopist maintains the snare cinched around half of the button of the PEG. The surgeon sees the tapered end of the PEG tube beginning to exit the abdominal wall and uses enough force to pull the tube through, placing the bumper resting loosely against the gastric mucosa and secures it with the bolster.
- Push Technique. Endoscopist inserts the G-tube over the guidewire. Both the endoscopist and surgeon hold tension on the wire while the G-tube is advanced into the stomach by the endoscopist and the tube is pushed until the tapered end can be grasped by the surgeon and pulled until the bumper rests loosely against the gastric mucosa and secured with the bolster until it is 2-3 mm above the skin.
Postoperative Considerations
- Gastrostomy tube is left to gravity postoperatively to allow for drainage and decompression of the gas insufflated during the procedure
- Tube feeds can be started 4 hours postoperatively if there were no concerns during the surgery. They should be started at a slow rate (10-20 mL/h) and increased by 10 mL every 6-8 hours until the goal rate is reached.
Postoperative Complications
- Clogged gastrostomy tube
- Dislodged gastrostomy tube
- Stoma leakage
- Fractured gastrostomy tube
- Gastrostomy tube infections
- Gastrostomy tube placed through bowel
- Gastric outlet obstruction
- Abdominal wall necrosis
- Buried bumper syndrome
- Tumor seeding