Large bowel obstruction occurs when there is a bowel obstruction distal to the ileocecal valve. Bowel obstructions have been documented as early as 1550 B.C. in the Papyrus.
Etiology
- Mechanical obstruction (dynamic)
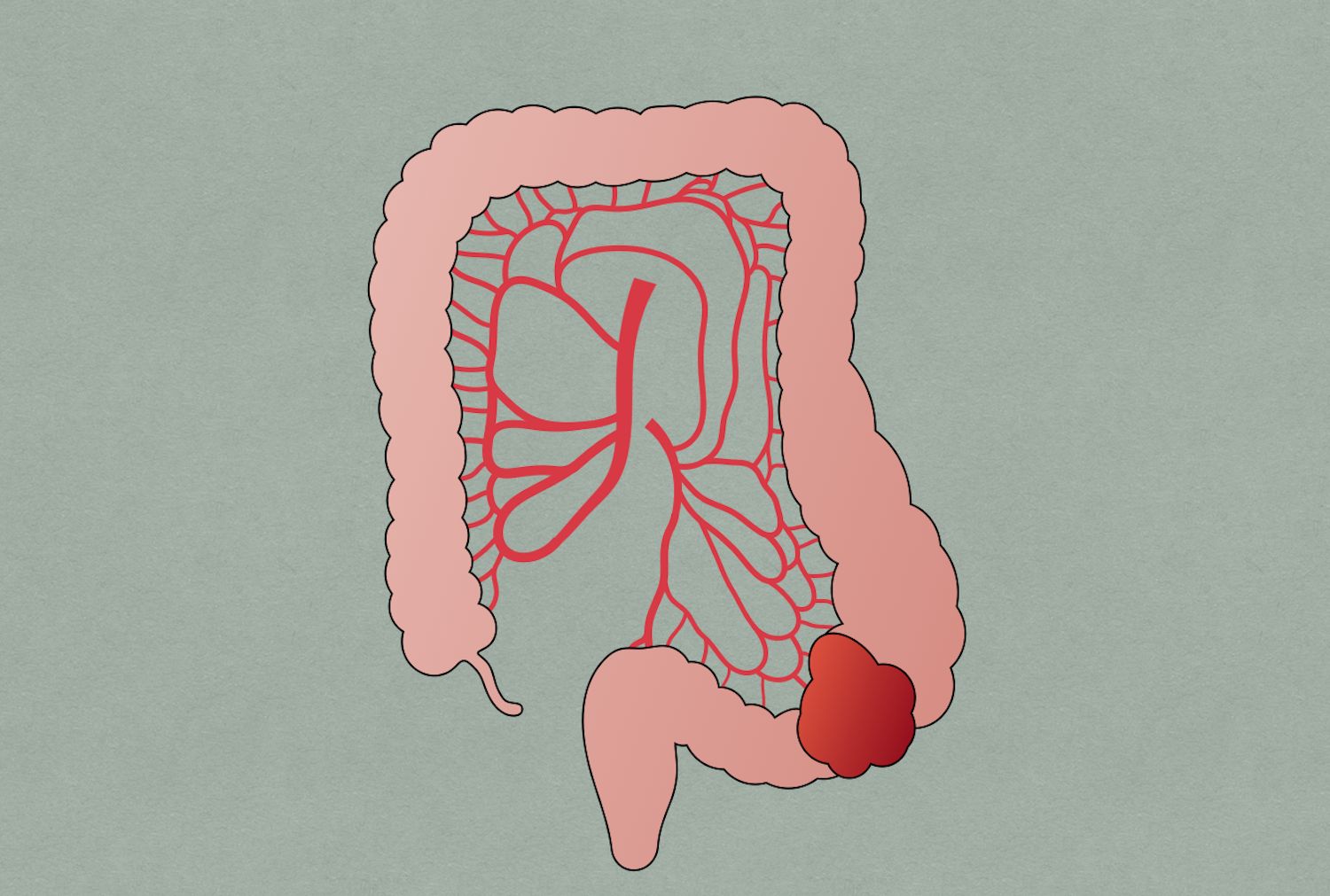
- Colorectal cancer is the most common cause in the U.S.
- Endoluminal causes
- Intrinsic mass
- Foreign body
- Bezoar
- Fecal impaction
- Mural causes
- Diverticular stricture
- Crohn disease stricture
- Ischemic stricture
- Radiation stricture
- Infectious
- Hirschsprung disease
- Extraluminal causes
- Sigmoid volvulus
- Cecal volvulus
- Hernia (i.e., inguinal, ventral, internal)
- Metastatic/intraabdominal tumor
- Abdominal abscess
- Retroperitoneal fibrosis
- Adhesions
- Functional obstruction (adynamic)
- Colonic pseudo-obstruction (Ogilvie)
- Toxic megacolon
- Paralytic ileus
History and Physical Exam
- Mechanical versus functional obstruction
- Mechanical obstruction
- Increased peristalsis
- Low-grade colicky pain
- Functional obstruction
- Abdominal distention
- Vague abdominal pain
- Mechanical obstruction
- Acute versus chronic obstruction
- Acute obstruction
- Rapid onset of pain
- Abdominal distention
- Abdominal tenderness
- Chronic obstruction
- Obstipation
- Abdominal distention
- Pencil-thin stools
- Intermittent abdominal pain
- Acute obstruction
Imaging
- Abdominal X-ray (location)
- Water-soluble and IV contrast-enhanced CT (location, etiology)
- Flexible endoscopy (diagnosis, biopsy)
Treatment
- Depends on etiology
- Surgery → for peritonitis, signs of perforation, ischemic bowel, patients that fail decompression for sigmoid volvulus, cecal volvulus, hernias, intussusception, cancer
- Endoscopic decompression (using rigid or flexible sigmoidoscope) → for sigmoid volvulus
- Steroids → for obstruction and active inflammatory bowel disease
- Drainage → for paracolic abscesses
- Endoscopic removal → for foreign body removal
- Stool softeners, laxatives, and manual disimpaction → for fecal impaction
Relevant Information
- Volvulus is responsible for ⅓ of cases
- Most common site is sigmoid colon
- Cecal volvulus can also occur
- Can occur at any portion of the colon not fixed to the retroperitoneum with elongated mesentery
- Closed-loop obstruction
- Occurs when proximal and distal parts of bowel are obstructed; colon becomes progressively distended with pressure increasing to the point of ischemic necrosis and perforation
- Potential for rapid deterioration with ischemia and bowel perforation
- Commonly encountered in cases of volvulus and strangulated hernias and in cases of obstructing colon cancers
- Pneumatosis intestinalis: air on the bowel wall; associated with ischemia and dissection of air through areas of the bowel wall
- Air in the portal system usually indicates significant infection or necrosis of the large or small bowel; often an ominous sign

- Large bowel = colon + rectum; 150 cm in length (roughly 5 feet)
- Covered with peritoneum; no mesentery
- Cecum
- Most common location for necrosis and perforation as it has the largest diameter
- Distends more under lower pressures and develops higher wall stress, per law of Laplace
- Law of Laplace: tension = pressure x diameter
- Risk of ischemic necrosis and perforation increases with diameter > 12 cm
- Ileocecal valve
- Where terminal ileum empties into cecum
- Thickened, nipple-shaped invagination containing circular muscle
- Appendix
- Extends from cecum 3 cm below ileocecal valve
- Blind-ending elongated tube 8 – 10 cm in length
- Ascending colon
- Begins at ileocecal junction and continues to hepatic flexure
- 15 cm in length (0.5 feet)
- Covered with peritoneum anteriorly and laterally
- Fixed against retroperitoneum by fascia of Toldt posteriorly
- Best mobilized along lateral peritoneal reflection by incising “white line of Toldt”
- Transverse colon
- 45 cm in length (roughly 1.5 feet)
- Covered by visceral peritoneum
- Greater omentum is attached at superior aspect; lifting upward with downward traction will reveal an avascular plane adjacent to the colon (most easily identified close to midline)
- Descending colon
- Begins at splenic flexure (where intestine loses its mesentery) to the sigmoid colon
- Splenic flexure
- Where transverse colon is flexed downward
- Suspended by four mainly avascular ligaments
- Phrenicocolic ligament
- Splenocolic ligament
- Renocolic ligament
- Pancreaticocolic ligament
- Sigmoid colon
- Begins at or below level of iliac crest where colon becomes completely intraperitoneal again
- Thicker and more mobile compared to descending colon
- When mobilizing, the mesenteric fold is the surgical landmark for underlying left ureter
- Ends at rectosigmoid junction (where colonic taenia confluence for form complete longitudinal muscle layer, and colon loses its mesentery)
- Splenic flexure
- 25 cm in length (0.82 feet)
- Commonly dissected along the line of Toldt from below and then enter lesser sac by lifting omentum above transverse colon
- Lesser sac (lesser peritoneal sac, omental bursa)
- Potential space that exists within the abdomen between the stomach and the pancreas
- Formed by greater and lesser omentum
- Lesser sac (lesser peritoneal sac, omental bursa)
- Smaller in diameter than ascending colon
- Begins at splenic flexure (where intestine loses its mesentery) to the sigmoid colon
- Meandering mesenteric artery (arc of Riolan, Moskowitz artery)
- Thick collateral vessel that courses closely to the base of the mesentery
- Connects SMA or middle colic artery to the IMA or left colic artery
- Presence suggests occlusion of one of the major mesenteric arteries
Complications
- Perforation
- Bowel necrosis, ischemia, gangrene
- Sepsis
- Electrolyte alterations
- Dehydration
- Death
Differential Diagnoses
- Megacolon
- Diverticulitis
- Small bowel obstruction
- Abdominal hernia